‘Having a Baby is Easier Than Getting a Root Canal’
 By Dr. Anthony Charles Caputo
By Dr. Anthony Charles Caputo
Regardless of your practice, as dentists, we have all heard the jokes and other comments identifying how terrible root canal therapy is for our patients. Despite the advancements in endodontics with respect to efficacy and efficiency in root canal therapy, patients still express their fear of this treatment approach. A study by Matsuura in 1989[i] identified that nearly 66% of systemic complications during dental treatment occur during extraction of teeth and root canal treatment. Interestingly, a recent report in the ADA Morning Huddle discussed an article from TIME Health[ii] that stated “Almost 40% of Americans are more anxious than they were at this time last year, according to a new American Psychiatric Association (APA) poll.” It is not uncommon for a person’s anxiety about personal issues and situations to manifest as increased fear and anxiety when presenting for dental treatment.
With increased fear and anxiety, it is important to understand and address this situation when a patient presents for endodontic treatment. This needs to be addressed as part of the initial evaluation of the patient. This includes completion and review of the medical history, collection of vital signs (minimally height, weight, blood pressure and pulse rate). The administration of drugs- local anesthesia or sedatives, requires that we obtain the patient’s weight. Height allows for the calculation of BMI which provides information regarding obesity and cardiovascular health. Following the medical evaluation, an anxiety assessment is completed. This is critical to identify how the patient feels about being in your office for treatment. This can be as simple as a visual analog scale that allows a patient to indicate how they are feeling (Figure 1). With identification of how your patient is feeling, you can begin the conversation about what you can do to help them have a successful appointment. Another key factor in assessing a patient’s fear or anxiety, is understanding the Dual Nature of Pain. The International Association for the Study of Pain (IASP) defines pain as, “An unpleasant sensory and/or emotional experience that is associated with actual or potential tissue damage”[iii] The keywords in this definition are “emotional” and “potential.” It is important to appreciate that pain is an emotional experience that is influenced by the potential for injury. This is often a critical assessment of the patient who presents with anxiety or fear to dental treatment.
Figure 1.
There are various strategies available to address anxiety and fear and we often already incorporate some or many of them in our current practices. Suggestion is a vital patient comfort approach and it involves creating an environment where our patients feel welcome and supported. Helpful and kind staff, a comfortable reception area, empathetic chairside manner are all methods of suggestion for the patient to understand you are going to take care of them in the best possible manner. Diagnosis of the condition with thorough explanation allows the patient to understand their situation and what needs to be done. Information empowers the patient and involves them in the treatment process. Profound local anesthesia administration is the most critical part of this process. Without profound anesthesia, the procedure will likely fail particularly for the anxious patient. This is an important point to understand with respect to sedation. The process of sedation is not a way to overcome the various strategies discussed. Sedation is an adjunct approach to facilitate the successful outcome of treatment. Patient selection and local anesthesia are the two key factors in the success of sedation for your patients.
Focusing on sedation, there are different approaches based on what is permitted by your state dental board. Nitrous Oxide-Oxygen Sedation (N2O-O2) is an excellent option for the mild to moderately anxious patient as well as an effective adjunct to other sedation approaches. Oral conscious sedation (OCS) provides an opportunity to improve sedation outcomes when combined with N2O-O2. Depending on the level of sedation being administered- minimal or moderate- there may be permitting requirements by your state dental board. Intravenous conscious sedation (IVCS) generally provides a broader sedation scope than OCS. Beyond minimal or moderate sedation administered by OCS or IVCS, there may be the opportunity to work with an anesthesia provider to administer deep sedation or general anesthesia.
With OCS, the most common drugs to administer are benzodiazepines which are good sedatives that also provide amnesia. Within this class of drugs, triazolam (Halcion) is a common and effective choice in combination with N2O-O2. Other commonly administered benzodiazepines are diazepam (Valium), alprazolam (Xanax) and lorazepam (Ativan). The caution with selecting an appropriate drug for any procedure is the planned length of time for the procedure and the duration of effect of the drug administered. For this reason, Halcion is an excellent choice understanding the duration of effect is typically in the 1-2 hour range. This effect can be enhanced with N2O-O2. Other drugs that have been administered successfully include zolpidem (Ambien) and zaleplon (Sonata). One challenge with OCS is the ability to titrate making this a less predictable approach than IVCS. Additionally, administering an oral drug sublingually is considered parenteral administration and may require a different permitting level. An approach to consider is administering the drug prior to the appointment, typically prior to sleep, to determine an appropriate effect. The challenge with OCS is not achieving the desired sedation effect. The best approach would be to ensure profound local anesthesia and consider increasing the level of nitrous oxide versus administering additional sedative drug. Ultimately, if OCS is not successful, plan on terminating the appointment and working with your patient to consider other sedation or anesthesia approaches for their procedure.
Anthony Charles Caputo, D.D.S., M.A., F.A.C.D., F.I.C.D., D.A.D.B.A., D.N.D.B.A, is dentist anesthesiologist and president, Southwest Dental Anesthesia Services. He is also a Fellow, American College of Dentists; Fellow, International College of Dentists; Diplomat, American Dental Board of Anesthesiology; and Diplomat, National Dental Board of Anesthesiology. He can be reached at anthony@swdas.com.
[i] Anesth Prog 1990, 36:219-228 Matsuura H. Analysis of systemic complications and deaths during dental treatment in Japan.
[ii] http://time.com/5269371/americans-anxiety-poll/
[iii] https://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1698&navItemNumber=576#Pain
Standing Firm in the Specialty Advertising Debate
 Last month, AAE president-elect Dr. Keith V. Krell and I had the pleasure of representing the AAE at the Dental Specialty Group meeting in Chicago. The leadership of each of the nine ADA-recognized specialties attends this biannual meeting to get an update from the ADA on topical issues and to discuss items of mutual interest among the dental specialties.
Last month, AAE president-elect Dr. Keith V. Krell and I had the pleasure of representing the AAE at the Dental Specialty Group meeting in Chicago. The leadership of each of the nine ADA-recognized specialties attends this biannual meeting to get an update from the ADA on topical issues and to discuss items of mutual interest among the dental specialties.
This year, the hot topic was again the issue of specialty advertising. The AAE is front and center in this debate, and we owe our executive director Ken Widelka a pat on the back for keeping this issue top of mind for our organization.
During the DSG meeting, Craig Busey, general counsel for the American Dental Association, presented an update precipitated by the 2017 5th Circuit Court decision in AAID vs. Parker that determined that advertising regulations permitting use of the term “specialty” only in connection with one of the ADA-recognized specialties violates First Amendment rights of dentists, such as implantologists, who have earned credentials from other certifying bodies. Following this decision, the American Board of Dental Specialties, an independent organization representing certifying boards in four areas of practice that are not currently recognized by the National Commission on Recognition of Dental Specialties and Certifying Boards, has sought to persuade state dental boards with similar regulations to completely deregulate specialty advertising, or be faced with a lawsuit.
It is the position of the AAE that regulating dental specialty advertising protects the public and therefore should be undertaken by state boards of dentistry. The AAE, together with the ADA and other specialty organizations, engaged outside legal counsel, Jack Bierig of Sidley Austin LLP, to develop a legal brief providing guidance to State Dental Boards on this matter, and outline a path forward for boards that would uphold regulations for advertising as a specialist while at the same time not risk violation of first amendment rights. Mr. Bierig’s legal brief outlining our position on misleading advertising is viewable here.
I will urge all members to get involved at your local level! While the AAE will continue to advocate on the national arena, these issues are also begging for local action. The reason we have been effective in states including Iowa (thank you, Dr. Krell), North Carolina (thank you, Dr. Levin) and Washington (my state), is largely because local members identified action taken by the ABDS to change state regulations. Get involved! Get on the update email list for your state boards or regulatory commissions. Stay attuned to your state AAE and ADA constituent societies to keep abreast of those issues affecting our specialty at the state and local level, then let us know what is happening. The general dentist groups having the greatest impact on expansion of the specialist definition are taking action at the state level, and those states where specialists are not responding are changing their rules — not always in our (or the public’s) best interest.
This is not a fight between general dentists and endodontists. It is an attempt by a limited group of “practice limited to” (primarily implantologists) dentists who would like to claim specialty status. Our position has long been that limiting claims of specialty status protects the public and maintains a level of public trust far superior to a “free-for-all” advertising push. Taken to the next level, would it be in the public’s interest to allow the advertising by non-dentists of dental or dental hygiene services?
We feel that public health and safety are best served when specialty status requires an approved residency at a CODA-accredited institution, not through unregulated accumulation of an arbitrary number of CE credits. Such forms of study are to be encouraged and appreciated. Many of our members have achieved distinction in groups such as the IADT and others through such courses, but they do not equate to the same knowledge and skill attained by completion of a CODA-approved residency.
The AAE stands firm in our position, and we will continue to keep you updated on this very important matter.
Virginia Advocacy Action Alert: Virginia State Board of Dentistry public comment open until September 5. The AAE strongly opposes deregulation of dental specialty advertising. Not regulating dental specialty advertising could harm patients. We strongly encourage our members in Virginia to voice their opinions on this matter to the Virginia State Board of Dentistry. Take action now!
Successful Week of Events Wraps in Chicago
 Endodontic educators, residents and corporate supporters gathered in Chicago last month for a series of AAE and Foundation for Endodontics-sponsored events. The Educator Workshop, Corporate Community Conference and APICES were held Aug. 24-25, giving all audiences an opportunity to interact and network with each other, as well as AAE leadership and staff.
Endodontic educators, residents and corporate supporters gathered in Chicago last month for a series of AAE and Foundation for Endodontics-sponsored events. The Educator Workshop, Corporate Community Conference and APICES were held Aug. 24-25, giving all audiences an opportunity to interact and network with each other, as well as AAE leadership and staff.
More than 30 corporate partners joined AAE leadership at the Corporate Community Conference, where “Trends in Endodontics” were a focus. After a welcome and overview from Marc P. Gimbel, D.M.D., chair, Corporate Relations Committee, and Mary T. Pettiette, D.D.S., president, AAE Foundation; Adriana Menezes, senior manager, Operations, Health Policy Institute, and Andrew Blatz, senior research and data analyst, Health Policy Institute, spoke.
AAE President Dr. Patrick E. Taylor also spoke on the “State of the AAE: Strategic Plan Update,” covering membership and global outreach, consumer awareness, and single standard for quality endodontics. Following the presentations, there was a reception with Educator Workshop attendees.
The AAE hosted 63 program directors during the 2018 Educator Workshop, “Assessing and Achieving Predoctoral Endo Competency.” Predoctoral directors worked through case studies after utilizing the Treatment Standard and Endodontic Competency White Papers to solve real-life scenarios. EAC Chair Dr. Craig Hirschberg moderated the conference. Sessions included “Competency: Is it in the eye of the beholder?” and “How does Licensure Impact Predoc Curriculum?”
The 15th annual APICES program also was held during this time, bringing 300 residents together to hear speakers on a variety of topics, including CBCT, clinical diagnoses and practice management, and to learn about the family of AAE organizations. All attendees had plenty of time to interface during meals, breaks and social events — such as an evening of dart games at downtown Chicago establishment Flight Club.
Residents seemed to enjoy the weekend-long experience, where they met their future colleagues, formed new relationships and learned about their specialty. A “sell-out” event year after year, APICES is completely free to all residents, providing registration, lodging and meals, as well as a travel stipend to offset the financial burden of attending.
Those gracious offerings are available because of the support provided by a variety of corporate sponsors.
Residents also showed their school spirit by providing videos representing their programs, which we compiled into a Welcome Video to kick off this year’s event. Watch it here, and view our full APICES photo album here.




WCDT 2018 a Successful, Unique Meeting in San Diego
 WCDT (World Congress on Dental Traumatology) 2018 was a first-of-its-kind event, jointly hosted jointly by the AAE and the International Association of Dental Traumatology. Held Aug. 15-18 in sunny San Diego, the four-day congress featured a whole host of prominent speakers – well-known experts in their respective fields.
WCDT (World Congress on Dental Traumatology) 2018 was a first-of-its-kind event, jointly hosted jointly by the AAE and the International Association of Dental Traumatology. Held Aug. 15-18 in sunny San Diego, the four-day congress featured a whole host of prominent speakers – well-known experts in their respective fields.
More than 40 world-renowned experts in dental and orofacial trauma representing 13 countries on 5 continents were present at the truly global event — along with nearly 600 attendees.
“The AAE is no stranger to global representation. While our name may start with ‘American,’ make no mistake, our membership represents 74 countries!” said AAE President Dr. Patrick E. Taylor in his opening remarks.
 Other highlights included JOE editor Dr. Ken Hargreaves’ “Regenerative Procedures for Immature Traumatized Teeth,” which described the three major steps in tissue engineering and how they apply to regenerating the pulp-dentin complex and communicated the clinical principles needed for regenerative endodontic procedures.
Other highlights included JOE editor Dr. Ken Hargreaves’ “Regenerative Procedures for Immature Traumatized Teeth,” which described the three major steps in tissue engineering and how they apply to regenerating the pulp-dentin complex and communicated the clinical principles needed for regenerative endodontic procedures.
Dental Traumatology editor Dr. Paul Abbott spoke on “Strategies to Reduce the Consequences of Impact Trauma to the Teeth,” which described the favorable and unfavorable responses of the pulp, peri-radicular and soft tissues to impact trauma.
 IADT President Dr. Nestor Cohenca’s “Diagnostic Imaging for Trauma Patients – Where Are We Today” communicated the clinical applications of current imaging technology in dental traumatology, reviewed the potential benefit of CBCT technology for diagnosis and treatment plan, and discussed the impact on treatment outcome and improved predictability.
IADT President Dr. Nestor Cohenca’s “Diagnostic Imaging for Trauma Patients – Where Are We Today” communicated the clinical applications of current imaging technology in dental traumatology, reviewed the potential benefit of CBCT technology for diagnosis and treatment plan, and discussed the impact on treatment outcome and improved predictability.
AAE Vice President Alan H. Gluskin’s presentation, “The Law: Critical Considerations for the Clinician and the Trauma Patient,” discussed the fundamental legal principles that apply to all patients regardless of the origin or nature of the dental condition and differentiated the basic steps of documentation to be taken in cases of dental trauma, in order to save teeth and avoid legal consequences.
Missed those four speakers? Not to worry, they will also be speaking at AAE19 in Montreal!
Over a dozen exhibitors comprised the exhibits portion of WCDT 2018. Our exhibitors and sponsors are an important part of this well-rounded experience for attendees.




2019-2020 Call for Committee Nominations
 Dear Colleagues,
Dear Colleagues,
As AAE president-elect, I am requesting your help identifying members to participate in the AAE through service on one of 17 standing committees. One of my most important responsibilities as president-elect is to develop a proposed slate of committee members that the Board will vote on at its April 2019 annual meeting. Please refer to aae.org/committees for a description of each committee.
Our standing committees are the backbone of our Association — every activity of the AAE takes shape at the committee level. The AAE is strong because of the dedicated, diverse and hard-working individuals who volunteer their time and talents.
There are a limited number of committee member positions available for three-year terms (2019-2022) and one-year resident member appointments. If you are interested in volunteering or suggesting colleagues that you think will serve the AAE effectively, please complete and submit the online Committee Nomination Form.
When completing the form, describe the work you or your colleague have done with the AAE, an AAE affiliate or state/local dental organizations, and why you and/or the person you are recommending would be an asset to the AAE. This information will be used in the appointment selection process, and all responses remain confidential.
If you have any questions, please contact Katherine Rouse, executive coordinator, by email at krouse@aae.org, or by phone at 312-266-7255, ext. 3005. All submissions are due by November 9, 2018.
Many thanks for your commitment to our Association. Working together makes the AAE the premier dental specialty organization it is today.
Sincerely,
Keith V. Krell, D.D.S., M.S., M.A.
AAE President-Elect
Staff Achievements
Congratulations to meeting services manager Justine Radies for attaining her CMP (Certified Meeting Professional), and to human resources manager Paul Young for his recent selection as winner of the Professional Development Faculty Distinguished Teaching Excellence Award from Northwestern University’s School of Professional Studies. You help our association shine!


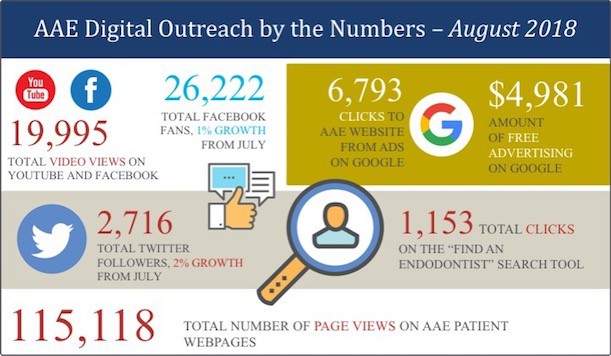
Digital Outreach By the Numbers – August 2018
Through the AAE website, social media channels, online advertising and digital resources, the Association educates the public about endodontics, helping them find specialists in their area, and provides shareable content for members and other dental professionals.
How Does Website Security (and HTTPS) Impact My Endodontic Practice?
By Jay Levine
![]() Sponsored Content
Sponsored Content
The Chrome web browser has launched a new update this July to alert visitors if the website they’re visiting is secure or “Not Secure”. This can be scary for patients looking to submit personal information on your website as identity theft affected 15 million people in 2017 alone.
Online security has become a huge priority for websites that collect HIPAA compliant patient data, require a password, conduct purchases (ie patient payments) or have private information that users may want to keep confidential. This is no surprise as HubSpot Research’s consumer survey found that 82% of website visitors will leave a website if it’s not secure. Considering that the Chrome Browser dominates 59% of the market share, your endodontic practice website will appear “not secure” to over half of your website visitors without being marked with HTTPS. This means having a non-secure website will cause 8 out of 10 patients to leave your site.
Building trust with new, referred and existing patients is extremely important and they want to feel confident in sharing their information with your practice. The best way to start building trust with patients is their first point of impression: your secured website.
What is HTTPS?
HTTPS stands for Hypertext Transfer Protocol Secure and Chrome marks your website as secure if “https” is at the beginning of your URL domain name. When you secure your website with HTTPS; you give your patients and referring doctors peace of mind to browse and submit personal information without the worry it’s being stolen or shared.
How Do I Make My Website Secure?
To implement HTTPS, you will need to contact your website hosting provider and get an SSL/TLS certificate. SSL stands for Secure Sockets Layer while TLS for Transport Layer Security and both encrypt information passed through the internet like transmitting passwords, patient data, credit cards or other personal information to and from your website’s server.
How Will I Know If My Site Is Secure?
Once you have an installed SSL/TLS certificate on your website server, your website will display HTTPS and the iconic lock symbol next to your web domain. Another additional benefit of HTTPS – the protocol is now a ranking factor in Google Search. Secure sites rank higher and are more visible on Google search results – another way in which SSL beneficially impacts your practice.
As the endorsed Website Design and Marketing Firm for the American Association of Endodontists, PBHS makes sure client websites are secure. Practices managed by PBHS are setup with complimentary HTTPS/SSL/TLS security. Please call PBHS with any questions at 1-800-840-5383 and mention you’re a member of the AAE.
Jay Levine is president and CEO of PBHS, the endorsed website design and marketing firm of the AAE.





