Maxillary Sinusitis of Endodontic Origin
 By Dr. Roderick W. Tataryn
By Dr. Roderick W. Tataryn
As endodontists, we take pride in our ability to accurately diagnose endodontic disease, diligently sleuthing out pulpal and periapical pathoses with careful clinical tests and radiographic imaging. We que into the slightest variations in percussion, palpation, thermal responses, and periodontal defects, and we notice tiny subtleties on radiographic imaging. But what happens when endodontic infection doesn’t look or feel like typical endodontic infection? What if endodontic disease, even in its most advanced, symptomatic stages, produces no dental pain, no clinical signs of swelling or sinus tracts, and no radiographic findings of ligament widening or osseous changes? And what if patients suffering with these advanced endodontic infections seek care from medical doctors who attempt treatments, sometimes for years, without ever recognizing the endodontic source? This situation is more common than perhaps many of us realize, occurring daily, all around us in our communities.
Endodontic infections that develop in the maxillary posterior teeth can easily spread into the maxillary sinuses causing pathological effects that frequently go unrecognized by both patients and clinicians alike. Failure to diagnose and properly manage these endodontic infections can lead to symptomatic sinus disease, defined as maxillary sinusitis of endodontic origin (MSEO).
Patients with MSEO experience common sinonasal symptoms, which include congestion, rhinorrhea, retrorhinorrhea, facial pain, and foul odor, yet they rarely experience typical endodontic symptoms. Thermal pain is normally absent because source teeth for MSEO are either necrotic or have failing endodontic therapy. Percussion tenderness is typically absent in MSEO because periapical infection is essentially draining into the sinus, eliminating pressure. For this same reason, swelling or intraoral sinus tracts rarely form.
Patients with sinonasal symptoms and without localized dental pain will often first seek care from their primary care physician or ear, nose and throat (ENT) specialist who may misdiagnose and treat MSEO as a rhinogenic sinus infection. Unfortunately, odontogenic sinus infections are often overlooked during routine ENT examinations and by radiologists reading sinus CT imaging. Sadly, current ENT clinical guidelines for the medical management of sinusitis offer no guidance in this area, making no mention of dental infections as a potential etiology for sinus disease despite abundant evidence in the medical literature of its high prevalence. Studies indicate that more than 40% of maxillary sinusitis cases are odontogenic, increasing to over 70% when maxillary sinus infections are unilateral. The American Association of Endodontists has recently published a Position Statement on Maxillary Sinusitis of Endodontic Origin as well as a Colleagues for Excellence issue to be widely distributed among our dental and medical colleagues in attempt to raise awareness of this condition and direct patients to endodontists who can properly diagnose and treat it.
Symptomatic or asymptomatic apical periodontitis near or in direct contact with antral mucosa will typically produce a localized mucosal tissue edema in the floor of the sinus termed periapical mucositis (PAM). PAM may progress causing partial or full obstruction of the maxillary sinus, which also can advance to involve other paranasal sinuses. Often no evident apical bony destruction occurs, especially when root apices protrude through the sinus floor, making many PAM or sinus obstructions difficult to recognize radiographically as having an endodontic source. A history of unilateral sinus infections, particularly if recurrent and/or associated with a patent ostium, is a strong indicator for possible MSEO. As with all endodontic diagnoses, a determination of etiology cannot be made based on radiographic examination alone. Careful clinical endodontic examination is imperative to confirm or rule out an endodontic source for mucosal abnormalities or sinusitis.
When diagnosing a possible endodontic etiology for sinusitis, the endodontist must look carefully for any teeth with pulpal necrosis and evaluate all prior endodontic treatments for possible failure in the suspected quadrant. Because MSEO is a bacterial disease, only teeth with an infected necrotic pulp or failing endodontic treatment will cause significant sinonasal disease or sinonasal symptoms. When examining maxillary posterior teeth with existing root canal treatment, one must carefully examine for any untreated or sub-optimally filled canals, inadequate core restorations, or leaking coronal restorations that may provide evidence of endodontic failure and a bacterial source for MSEO.
The objectives for treatment of MSEO are removal of the pathogenic microorganisms, their by-products, and pulpal debris from the infected root canal system that are causing the sinus infection and preventing reinfection. Use of systemic antibiotics to manage MSEO should follow the guidelines set forth in the AAE Guidance on the Use of Systemic Antibiotics in Endodontics. Apart from spreading infections, antibiotic therapy is unwarranted in the treatment of MSEO and ineffective as a definitive solution. While antibiotic therapy may offer temporary relief of symptoms by improving sinus clearing, their sole use is inappropriate without definitive debridement and disinfection of the root canal system.
Similarly, surgical intervention of the maxillary sinus that is focused strictly on removing diseased sinus tissue and establishing drainage is inadequate if the endodontic component is neglected. Although these procedures are performed by ENT surgeons with the goal of re-establishing sinus aeration and drainage, and may provide relief of some symptoms, it is well documented that neglecting the dental etiology and focusing only on medical and surgical therapies of the ostiomeatal complex (OMC) will not resolve MSEO.
The dental literature provides numerous case reports showing full resolution of MSEO following endodontic treatment. It should be noted, however, that endodontic treatment alone may not resolve all cases of MSEO, therefore clinical and radiological follow-up is essential as concomitant management of the associated rhinosinusitis by an ENT specialist may be necessary in some cases. Improved communication and collaborative referral relationships between general dentists, endodontists, and ENT surgeons is essential to achieve the best outcomes for patients suffering with MSEO.
MSEO is fundamentally an endodontic infection manifesting in the maxillary sinus. It is up to us as endodontists to bring awareness to the medical community of this underappreciated and frequently unrecognized disease process. After all, MSEO is endodontic disease.
Works Cited
Longhini AB, Ferguson BJ. Clinical aspects of odontogenic maxillary sinusitis: a case series. Int Forum Allergy Rhinol 2011;1:409–415.
Patel NA, Ferguson BJ. Odontogenic sinusitis: an ancient but under-appreciated cause of maxillary sinusitis. Curr Opin Otoloaryngol Head Neck Surg 2012;20:24-28.
Pokorny A, Tataryn R. Clinical and radiologic findings in a case series of maxillary sinusitis of dental origin. Int Forum Allergy Rhinol 2013;3:973-979.
Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, et al. Clinical practice guideline (update): Adult sinusitis executive summary. Otolaryngol Head Neck Surg 2015;152:598–609.
Fouad AF, Byrne BE, Diogenes AR, et al. AAE Guidance on the Use of Systemic Antibiotics in Endodontics. American Association of Endodontists Position Statement 2017:1-8. Available at: https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/aae_systemic-antibiotics.pdf .
Tataryn RW, Lewis MJ, Horalek ML, et al. Maxillary Sinusitis of Endodontic Origin. American Association of Endodontists Position Statement 2018:1-11. Available at: https://www.aae.org/specialty/wp-content/uploads/sites/2/2018/04/AAE_PositionStatement_MaxillarySinusitis.pdf .
Our Future is Bright
 Last month’s President’s message outlined changes to specialty status that can negatively affect the practice of endodontics. This month, I would like to present a more positive perspective, my belief that the future of endodontics looks great. I say this from a view of 34-plus years as a member of the AAE. When I was applying for residency, I was advised that endodontics was a dying specialty. I must admit that no endodontists told me that, but it has been a background sentiment as long as I have been associated with the specialty. Over that time endodontics has done quite well and continues to be a major factor in improving the health of our patient population.
Last month’s President’s message outlined changes to specialty status that can negatively affect the practice of endodontics. This month, I would like to present a more positive perspective, my belief that the future of endodontics looks great. I say this from a view of 34-plus years as a member of the AAE. When I was applying for residency, I was advised that endodontics was a dying specialty. I must admit that no endodontists told me that, but it has been a background sentiment as long as I have been associated with the specialty. Over that time endodontics has done quite well and continues to be a major factor in improving the health of our patient population.
We are now the specialty associated with saving teeth and have been advocating for years that patients should retain their natural dentition for as long as they can. We can provide root canal therapy faster, better and with greater comfort because the equipment, clinical techniques and materials have improved tremendously (does anyone remember micro burs for root end preps?). The resulting raise in the cost of doing business has been a burden, but one not easily shouldered by non-endodontists. Root canal therapy has become more complex, demanding and difficult over the years to the point where the non-endodontists can’t keep up. That puts us farther out ahead in delivering care in an efficient, successful manner.
I think that there is a consensus that we cannot do all of the root canals out there, but we should be doing the difficult, complex cases. Let’s train non-endodontists and dental students to do the routine, straightforward endodontics if they wish, but also teach them to refer the rest to a specialist and let us sweat the difficult cases. Certainly do not condone the extraction of teeth because it would be “easier.”
In August, I attended the APICES meeting in Chicago and was much impressed with what I saw of the future leaders of our specialty. The meeting is designed and run by residents and the RNPC (Resident and New Practitioner Committee) with great support from AAE Headquarters staff. The meeting was terrific. Three hundred residents got to hear great speakers on the latest in clinical techniques, equipment, materials and practice management. The biggest complaint I heard was that non-member residents had difficulty signing up. Please take note, program directors: advise your new residents to join the AAE when coming in as we have a lot to offer! We continue to scale up the attendance capacity (50% increase over the last two years) and will make it better and better as we go forward. Judging by what I saw in the lectures, in the exhibit spaces and at social gatherings, the current residents will be coming into the workforce much better prepared than my cohort.
My admonition to current residents is to keep moving forward. Let’s make endodontics better and position the specialty well for next 10, 20, 30 years. I hope that in 2051 there will be better tools that make today’s techniques seem as outdated as micro head handpieces; and endodontists are still the go-to specialists for saving teeth.
Lastly, a message to all AAE members: in the spirit of looking ahead, I want to make mention of a couple of very important educational events on the horizon. They are our upcoming Insight Track Workshops: 1) Surgery Workshop, held Nov. 2-5, 2018, in Chicago (attendees have a choice between either Nov. 2-3, or 4-5), and 2) Cone Beam Computed Tomography, occurring Jan. 24-26, 2019, in Lake Tahoe, Calif. — a perfect opportunity to combine learning with vacation, even if you don’t ski! Space for both Insight Track programs is very limited, so be sure to register before these events sell out.
Congratulations to 2018 Endodontic Educator Fellow Dr. Annie Shrestha
 The Foundation for Endodontics firmly believes the strength of the specialty starts from strong educational opportunities. One way the Foundation works hard to keep the specialty relevant and on the cutting edge is by its commitment to ensuring specialists teach endodontics at dental institutions across the United States and Canada. The Endodontic Educator Fellowship Award is one of the Foundation’s flagship funding opportunities and directly addresses this issue.
The Foundation for Endodontics firmly believes the strength of the specialty starts from strong educational opportunities. One way the Foundation works hard to keep the specialty relevant and on the cutting edge is by its commitment to ensuring specialists teach endodontics at dental institutions across the United States and Canada. The Endodontic Educator Fellowship Award is one of the Foundation’s flagship funding opportunities and directly addresses this issue.
The award provides funding to individuals who commit a minimum of five years to a full-time* academic career in endodontics at a dental school that is accredited by or has a reciprocal agreement with the Commission on Dental Accreditation of the American Dental Association. Recipients receive $50,000 a year, for five years; up to $250,000 is available per recipient.
Annie Shrestha, B.D.S., M.Sc., Ph.D., FRCD(C), assistant professor at the Faculty of Dentistry, University of Toronto impressed the committee with her poise and distinguished approach to education. Dr. Shrestha feels strongly that her tenure track appointment at Toronto has given her the kick-start needed to develop an interlink between dental education and meaningful contributions to improving healthcare. During her time as a Ph.D. student and endodontic resident, Dr. Shrestha gave back to the endodontic community in the way of publications, presentations and AAE committee service.
“I derive enormous satisfaction from knowing that as an educator, I have an opportunity to play a significant role in training endodontists who will excel in and cherish their profession,” said Dr. Shrestha.
Dr. Shrestha brings forward a unique blend of talent, with a Ph.D. (nano-materials and translational research) and post-doctoral training and clinical training in endodontics. In the long run, Dr. Shrestha plans to develop her research niche towards unraveling the effect of metabolic diseases on immune responses of chronic infection, and how immune-modulation can be utilized to achieve better therapeutics.
The Foundation for Endodontics is proud to name Dr. Annie Shrestha the 2018 Endodontic Educator Fellow. The Special Committee and the Foundation’s Board of Trustees feels confident she will serve as a strong leader and bring remarkable things to her students and the specialty, for years to come.
*Full time as defined by the employer institution.
Life Member Dr. Bruce Seidberg Elected to AADB Board
 Congratulations to life AAE member Dr. Bruce Seidberg for being elected secretary for the American Association of Dental Boards at the recent AADB meeting in Chicago.
Congratulations to life AAE member Dr. Bruce Seidberg for being elected secretary for the American Association of Dental Boards at the recent AADB meeting in Chicago.
Dr. Seidberg has a long history with the AAE, including serving as a trustee from 1989-1992 and secretary-treasurer from 1991-1992 of the AAE Research and Education Foundation (which was later renamed Foundation for Endodontics). He served on the AAE Board of Directors from 1993-1996 and 1999-2002. In 2002, he was presented with the AAE President’s Award.
Dr. Seidberg is a past president of the American College of Legal Medicine and of the Onondaga County (NYS) Dental Association. In 2013 he was awarded the ACLM Gold Medal for services to Dentistry and Law. He was recently Chairman of the New York State Board for Dentistry.
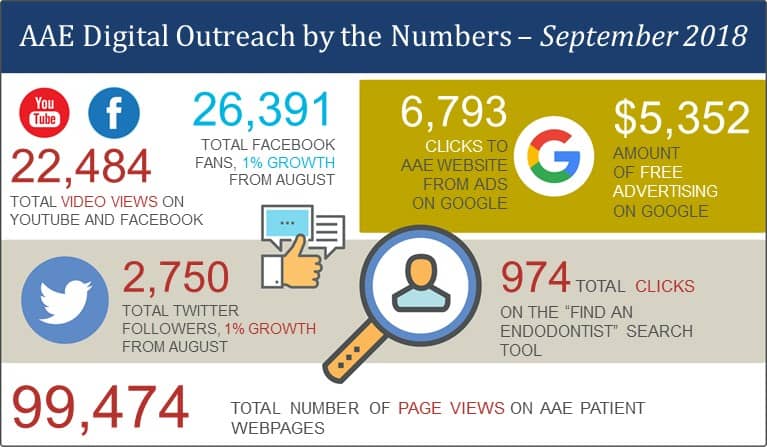
Digital Outreach by the Numbers – September 2018
Through the AAE website, social media channels, online advertising and digital resources, the Association educates the public about endodontics, helping them find specialists in their area, and provides shareable content for members and other dental professionals.
How to File a Disability Income Insurance Claim
By D. Scott Fehrs, ChFC®
 Insurance is one of those things in life that you buy and hope to never use. Disability income insurance is one of the primary insurances that you really hope not to have to use. And yet, should that day ever come, you’ll be happy you bought it.
Insurance is one of those things in life that you buy and hope to never use. Disability income insurance is one of the primary insurances that you really hope not to have to use. And yet, should that day ever come, you’ll be happy you bought it.
Pretty much everyone knows someone who was disabled through accident or illness, and – whether temporarily or permanently – was unable to return to work. When that happens, first is the immediate shock of what happened to you. “Will I be OK? Can I go to work again? How will I provide for my family?”
Assuming that you had the foresight to buy disability income insurance, the next question is “Will the insurance company pay my claim?” To some degree, every claimant experiences the dread of not knowing if his or her claim will be accepted.
Once you file your claim, the insurance company will need to ascertain a number of things about you. They need to know your occupation at the time of the disability, the nature of your disability, and your income. As simple as this may seem, a lot of energy goes into giving them this information so that they can produce an answer for you.
Being better educated about the claims process could put you in a better place emotionally, and help you move through this time efficiently. To help manage your anxiety, I thought I’d put together a few concepts you will need to understand:
Occupation
The insurance company cares about your occupation at the time of disability. Say you bought your insurance policy when you were an oral surgeon, but now you are a consultant to a national implant company. Well, this change may make a difference as to how the company evaluates your claim. (By the way, how an insurance provider defines the word ‘occupation’ is one of the most important things a dentist needs to understand about a disability income policy.)
Elimination Period
The elimination period is the period of time that needs to lapse before the insurance company starts accruing your benefits. Many people mistakenly believe that this is when you start receiving your checks – it’s not.
A personal disability policy will typically have a 90-day elimination period, though other options exist. A business overhead policy may have a 30-, 60- or 90-day elimination period.
If you have a 90-day elimination period it’s important to realize that you’re not going to start receiving checks on the 90th day after your disability. You will start accruing benefits after 90 days with payments usually beginning a short time thereafter.
Due Diligence
It’s easy to be cynical and say that insurance companies do not pay claims. They absolutely do pay appropriate claims, they just need to thoroughly research your claim. This process is known as due diligence.
Due diligence includes getting statements from your attending physician. It also includes getting your tax returns. While this may feel highly invasive, it has nothing to do with the insurance company being ‘nosy.’ The statements from your medical providers help the insurance company determine the nature of your disability.
Your financial statements help provide a picture of your financial health. Some companies will look back as far as five years to determine your income. This can be advantageous for you. We saw this in 2008 and 2009 when many clients’ incomes were down and our clients could look back as far as 2005 to determine income. So you see, it’s not necessarily bad to give them the information they seek.
Establish your cash reserve – NOW.
You’d be surprised at how many (even high-earning people) don’t have adequate cash reserves. By now you will have figured that if an insurance company has a waiting period of 90 days before they even start looking at your paperwork, realistically, you’re not getting a check until at least 120 or 130 days after your disability event. This represents at least four months that you may need to pay for your ongoing expenses out of pocket.
You should have a minimum of 6 months’ worth of expenses in cash. Ideally, 9 months or even a year’s worth would give you peace of mind that you’re covered in the event of an unexpected mishap.
Work with your ‘support team’
Make sure your broker is experienced in handling claims like yours. Your broker could be your chief advocate during the claims process. Also, I can’t stress enough how important it is to work with your accountant, doctor’s office, and everyone else who is going to help you as you go through this process.
Let everyone on your support team know that time is of the essence. The faster they move to give the insurance company the information it needs, the faster you’ll have your check in hand. Time is money!
If you follow these steps, you should be in good shape. Good luck with your claim.
###
18-001
D. Scott Fehrs is chief executive officer, Treloar & Heisel, Inc. Learn more at www.treloaronline.com.
Treloar & Heisel and Treloar & Heisel Risk Management are divisions of Treloar & Heisel, Inc. Insurance products offered through Treloar & Heisel and Treloar & Heisel Risk Management. Treloar & Heisel, Inc. does not offer tax or legal advice.





