Case Treatment Plan: February 2018
By Alex C. Moore, D.M.D.
This is a case study of a 55-year-old female that was presented to the Marquette University School of Dentistry. She was referred to the post-graduate endodontic clinic for a consultation of tooth 14. The patient was asymptomatic on 14 and she was treatment-planned for a fixed partial denture at 12-14. Teeth 12 and 14 had tested normal to percussion, palpation, and probing depths were under 3 mm. The patient reported having the root canal therapy on tooth 14 overseas more than 10 years ago and has never had an issue with it. No historical radiographs were available for comparison.
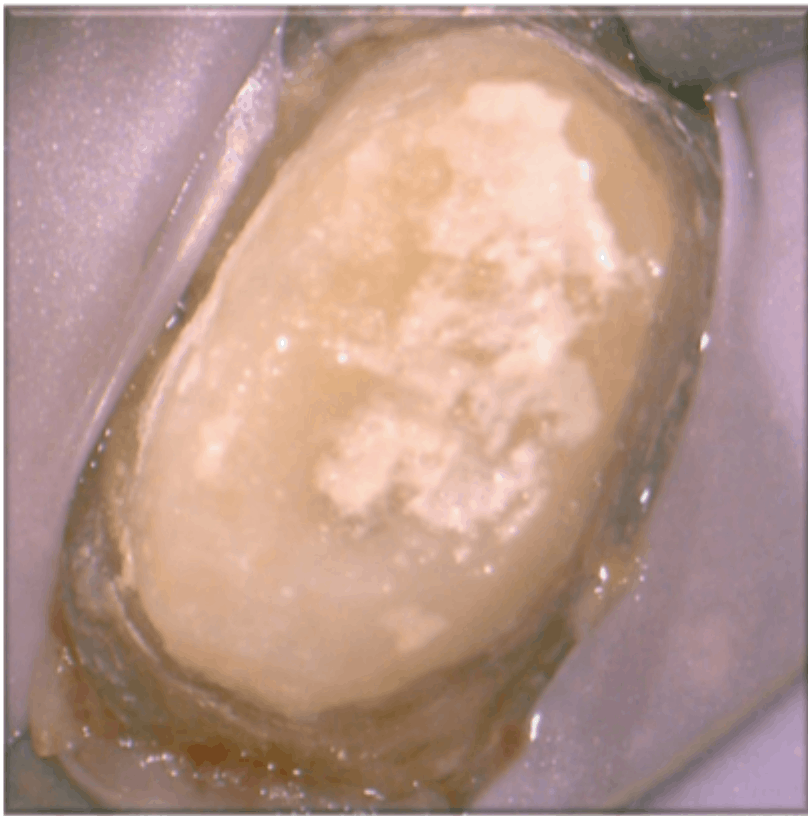
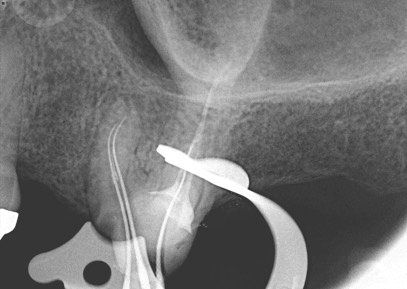
The patient’s medical history was non-contributory. Tooth 14 had a temporary crown recently placed by an undergraduate dental student. Upon radiographic evaluation of the periapical radiographs, it was determined that each canal was under-filled. The palatal root had a large, pre-existing fiber post and a composite core buildup was present.
A radiolucency on the MB root was suspected in the periapical imaging. A limited-field CBCT was captured. A moderate-sized periapical hypodensity confined to the mesiobuccal root was visualized with CBCT imaging. This hypodensity was consistent with a lesion of endodontic origin. The distal and palatal roots appeared to have an intact lamina dura, in particular, a normal periapical area.
Based on this information, the diagnosis of tooth 14 was:
Dx: Tooth 14 Previously Treated with Asymptomatic Apical Periodontitis.
A thorough conversation was had with the patient regarding the presence of apical bone loss most likely of endodontic origin. It was explained to the patient that because we do not have historical radiographs, we cannot confirm how long the hypodensity has been present. The unknown prognosis of 14 in terms of, if it would ever cause her symptoms with or without treatment, also was explained. In the patient’s eyes, the goals of the procedure had been met; she has been asymptomatic and able to retain her tooth.
Based on the examination, and treatment plan of having a new FPD placed from teeth 12-14, I recommended a selective retreatment of the MB and DB roots on tooth 14. After confirming radiographically that the palatal root apex appeared within normal, I felt that the process of removing the fiber post out of the palatal root could create more harm than benefit. The patient was explained the risks/benefits/costs of doing such treatment compared with no treatment and agreed to the treatment plan of selective retreatment of tooth 14. The patient was also made aware that if she developed a lesion that needed treatment on the palatal root, she would not be charged for that treatment.
Appointment 1:
- Clinical and radiographic examination
- Anesthesia and isolation with rubber dam
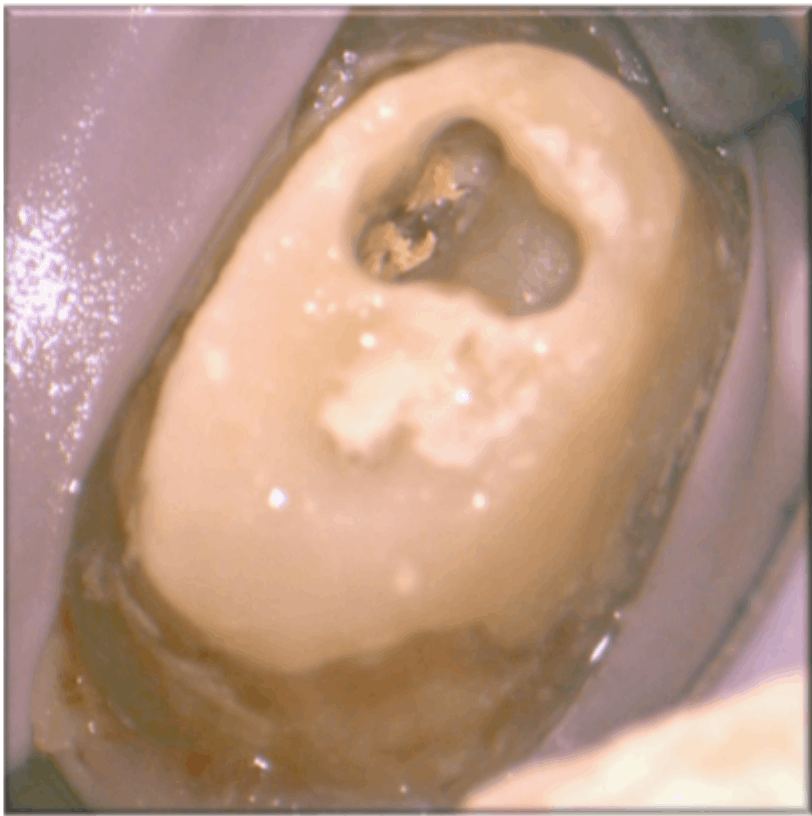
- Limited occlusal access, directed toward buccal canals (CBCT guided)
- Removed gutta-percha of MB, DB and MB2 canals using hand files and chloroform
- Achieved patency on all three canals and established working lengths
- Thorough disinfection with 5.25% NaOCl and 17% EDTA
- Placed CaOH and temporized using cavit
Appointment 2:
- Anesthesia and isolation with rubber dam
- Re-access canal spaces
- Thorough disinfection with 5.25% NaOCl and 17% EDTA
- Continuous wave obturation with gutta-percha and BC sealer
- Restored using composite
The patient remained asymptomatic at the second appointment and at the three-month follow-up appointment. At the follow-up, the tooth had been restored with a fixed partial denture. The three-month follow-up CBCT demonstrated evidence of healing. The patient is scheduled for future follow-up appointments to evaluate long-term success.
If you have a Case Treatment Plan or Case Challenge you would like to submit for publication, please contact Allison Houle.