Hindsight is 20/20 and Second Chances are Divine
By Mary Um, D.M.D., M.S.
The following is a case study supplied by Dr. Mary Um, describing what ultimately became a non-surgical retreatment case.
An 82-year-old white female presented with chief complaint of “I still have a dull ache in that tooth six months after I had the root canal done.” The patient reports mild throbbing ache from tooth no. 15. No swelling or deep probing depths noted. Occlusion was checked and no interferences or other malocclusion noted.
Medical history: She is an ASA II patient. She reports having a heart condition, diagnosed with A-fib 2010 and an adverse reaction to epinephrine. She is currently seeking treatment for Sciatic nerve pain that keeps her up at night. She denies any history of surgeries and does not take any medications even with the sciatic nerve pain. The patient also reports allergies to sulfa medications and iodine dye.
Hx Current Illness: I first completed a root canal therapy on tooth no. 15. Pre-op diagnosis was symptomatic irreversible pulpitis and symptomatic apical periodontitis. She initially reported moderate to severe pain to temperature changes and biting pain. After the root canal she did not return to me with any complaints for six months. When I saw her again after six months, patient reports that the nature of pain has changed since the root canal has been completed but has not resolved. Now, the pain is mild, dull and achy. Her general dentist restored the tooth with a large composite build-up including the distal cusps but decided not to place a full cuspal coverage restoration until symptoms were completely gone. The patient spent her winter in Florida and had an endodontist and a periodontist in Florida evaluate the tooth clinically and radiographically but no one could come up with a diagnosis. According to the patient, both specialists did not find anything wrong with the tooth and told her it was possibly fractured and if the symptoms do not go away to extract tooth no. 15. When she returned to the north after the cold months, her general dentist took tooth no. 15 out of occlusion but the dull ache did not resolve.
Clinical findings: Probing depths were 3-4 mm circumferentially. No isolated probing depths were noted.
| 12 | 14 | 15 | |
| Cold | – | + | – |
| Palp | – | – | + |
| Perc | – | – | + |
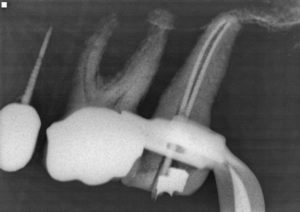
Radiographical findings: Periapical radiographic did not reveal any abnormalities. Good quality obturation noted. CBCT scan shows no isolated bone loss consistent with subosseous cracks. It did reveal the B canal was not centered. It suggests that there is a possible mid-root split in the B canal. Remainder of CBCT scan is unremarkable.
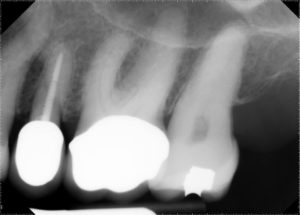
Pre-op PA from 2018
Master cone PA from 2018

Post-op PA from 2019
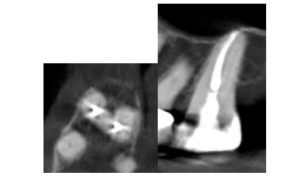
Post-op CBCT
I ended up performing a non-surgical retreatment on no. 15. I found a mid-root split in the M root. I treated the tooth in two appointments just to see if her symptoms subsided. Patient reported all symptoms resolved as soon as I retreated the tooth.

Final PA after non-surgical retreatment
We all make mistakes; being a new provider I am especially humbled every day. Hindsight is 20/20. Now looking back, maybe there was a shadow of a second canal. I’m grateful my patient was willing to let me give it a second shot. In her words, “that’s why it’s called practice of dentistry.” I thank her physician husband for sharing that with her through his career.
This case reminded me of an article I read in residency. Ee, et al. Comparison of endodontic diagnosis and treatment planning decisions using cone-beam volumetric tomography versus periapical radiography. J Endod. 2014 Jul;40(7):910-6. doi: 10.1016/j.joen.2014.03.002. Epub 2014 Apr 16. In this study, the researcher showed that “preoperative CBVT imaging provides additional information when compared with preoperative periapical radiographs, which may lead to treatment plan modifications in approximately 62% of the cases (Ee).” Without a CBCT scan, all providers who were involved in the case assumed there was a fracture in the offending tooth. Two endodontists were involved in the case separately and neither one could see the DB canal on any of the PA radiographs.
This case clearly demonstrates the superiority of 3-dimensional imaging over 2-dimentional imaging. It also showcases how much more I have to learn as an endodontist.




