AI-Powered Clinical Decision Support Tools in Endodontic Education
By Keith R. Boyer, DDS
The concept of Artificial intelligence (AI) has existed for many years, but recent advances in technology, such as ChatGPT, have brought AI to the forefront of our daily lives. This explosive growth of technology has a profound opportunity to reshape medicine, research, and education. Machine learning, a subset of AI with particular relevance to dentistry, trains models to recognize patterns in data such as images: This has allowed for computer assistance in detecting various findings in radiographic images with a high degree of accuracy.1 AI-powered clinical decision support (CDS) tools based on machine learning are used in dentistry to efficiently aid clinicians in diagnosis, to process insurance claims, and more recently, to assist in dental education.2
“You don’t know what you don’t know.”
As the above adage goes, AI models and dental students alike cannot find what they are not taught to see. For AI software, the output depends on how it was trained and the algorithms employed in decision-making, and this process is not always readily transparent.1 Therefore, clinicians should exercise caution interpreting results from AI CDS tools. When teaching radiographic interpretation to dental students, faculty describe features of caries and periapical radiolucent lesions (PARLs) and provide sample illustrations. Students then build upon this foundational knowledge through clinical encounters. AI CDS tools can augment this experience with the simple click of a button, showing students what to look for in an unlimited number and variety of clinical examples (Figure 1), helping to bridge the gap between novice and expert dentist. This technology may also assist in patient education and case acceptance by giving patients with untrained eyes the ability to clearly see areas of concern.
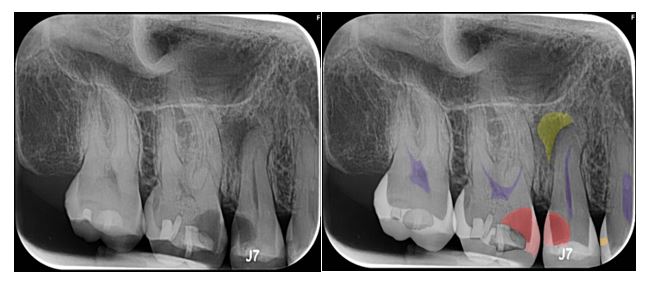
Figure 1: First image, a periapical radiograph without AI CDS tools. Second image, a periapical radiograph in which Overjet AI software highlights caries, periapical radiolucency, and the pulp space of each tooth shown.
As part of their training, students are instructed to interpret the entire image, but PARLs may be missed due to lack of a related chief complaint or because of the difficulty identifying such lesions in 2D imaging due to overlapping structures.3 Busy faculty may overlook such findings as well. One study of radiographic periapical diagnosis of posterior teeth showed a sensitivity of 65% and a specificity of 78%, suggesting that many PARLs go undetected or are misdiagnosed as false positives by clinicians.4 AI tools trained to detect PARLs in 2D radiographs and 3D CBCT imaging may result in greater accuracy than unaided practitioners. A recent systematic review with meta-analysis of AI detection of PARLs in 2D and 3D imaging showed pooled sensitivity of 92.5% and specificity of 85.2%.5 Another found pooled sensitivity of 94% and specificity of 96%.6 While this is aggregate data of PAs and CBCTs, these examples suggest that artificial intelligence may improve practitioners’ ability to recognize PARLs more consistently. One potential benefit of AI CDS tools in dental education is to act as a failsafe and quality assurance to identify undocumented PARLs and possibly address instances of untreated disease.
On the other hand, endodontic residents will be faced with referring dentists who are using AI CDS tools, and they may be pressured to “treat the radiograph.” When a commercial AI-based platform was used to evaluate outcomes of endodontic treatment, the software resulted in lower specificity compared to clinicians, which if used without checking could result in overdiagnosis and unnecessary retreatment.7 Endodontic residents need to be prepared to discuss why this technology is not foolproof. To most efficiently implement such software, one must learn its limitations, understanding the strengths and weaknesses.
It is crucial that educators teach students to use technology responsibly. As dental students graduate and enter modern practice, the hope is they do not blindly trust what AI software tells them. Instead, they should utilize it with a critical eye for its intended purpose, to support and assist diagnosis. Large carious lesions or the presence of PARLs should alert the clinician to evaluate the pulpal status of teeth in question. It should not be assumed that every tooth with PARL needs endodontic therapy. Practitioners can use AI CDS systems to assist in the screening of images but must integrate all available diagnostic information and clinical judgment to establish periapical diagnoses. An educator’s responsibility is to ensure that graduates will be prepared to practice safely and with confidence in this world of ever-changing technology.
References
- Arsiwala-Scheppach LT, Chaurasia A, Muller A, Krois J, Schwendicke F. Machine Learning in Dentistry: A Scoping Review. J Clin Med. 2023; 12(3).
- Aminoshariae A, Nosrat A, Nagendrababu V, Dianat O, Mohammad-Rahimi H, O’Keefe AW, et al. Artificial Intelligence in Endodontic Education. J Endod. 2024; 50(5): 562-578.
- Endodontists AAo. Competence in the Diagnosis of Endodontic Treatment. 2017.
- Bohay RN. The sensitivity, specificity, and reliability of radiographic periapical diagnosis of posterior teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000; 89(5): 639-42.
- Sadr S, Mohammad-Rahimi H, Motamedian SR, Zahedrozegar S, Motie P, Vinayahalingam S, et al. Deep Learning for Detection of Periapical Radiolucent Lesions: A Systematic Review and Meta-analysis of Diagnostic Test Accuracy. J Endod. 2023; 49(3): 248-261 e3.
- Pul U, Schwendicke F. Artificial intelligence for detecting periapical radiolucencies: A systematic review and meta-analysis. J Dent. 2024; 147: 105104.
- Allihaibi M, Koller G, Mannocci F. Diagnostic Accuracy of a Commercial AI-based Platform in Evaluating Endodontic Treatment Outcomes on Periapical Radiographs Using CBCT as the Reference Standard. Journal of Endodontics. 2025; 51(7): 898-908.e8.
Keith R. Boyer, DDS is an Associate Professor and Coordinator of Endodontic Care at Western University of Health Sciences, College of Dental Medicine in Pomona, CA. He has no conflicts of interest to report.
Disclaimer
The views and opinions expressed by authors are solely those of the authors and do not necessarily reflect the official policy or position of the American Association of Endodontists (AAE). Publication of these views does not imply endorsement by the AAE.
