Case Challenge
By Dr. Adam Gluskin
Case History: A 56 year old male patient was referred for evaluation of tooth #7 and #8. He is asymptomatic, but his general dentist referred him after observing a buccal sinus tract over tooth #7.
Medical history: Non-contributory, ASA I
Medications: None
Allergies: NKDA
HPI: The patient reports RCT #8 and crowns on #8 and #9 following a bike accident over 20 years ago. The teeth have been asymptomatic ever since, but the patient reports a "bump" in the gums developing on and off over the past year.

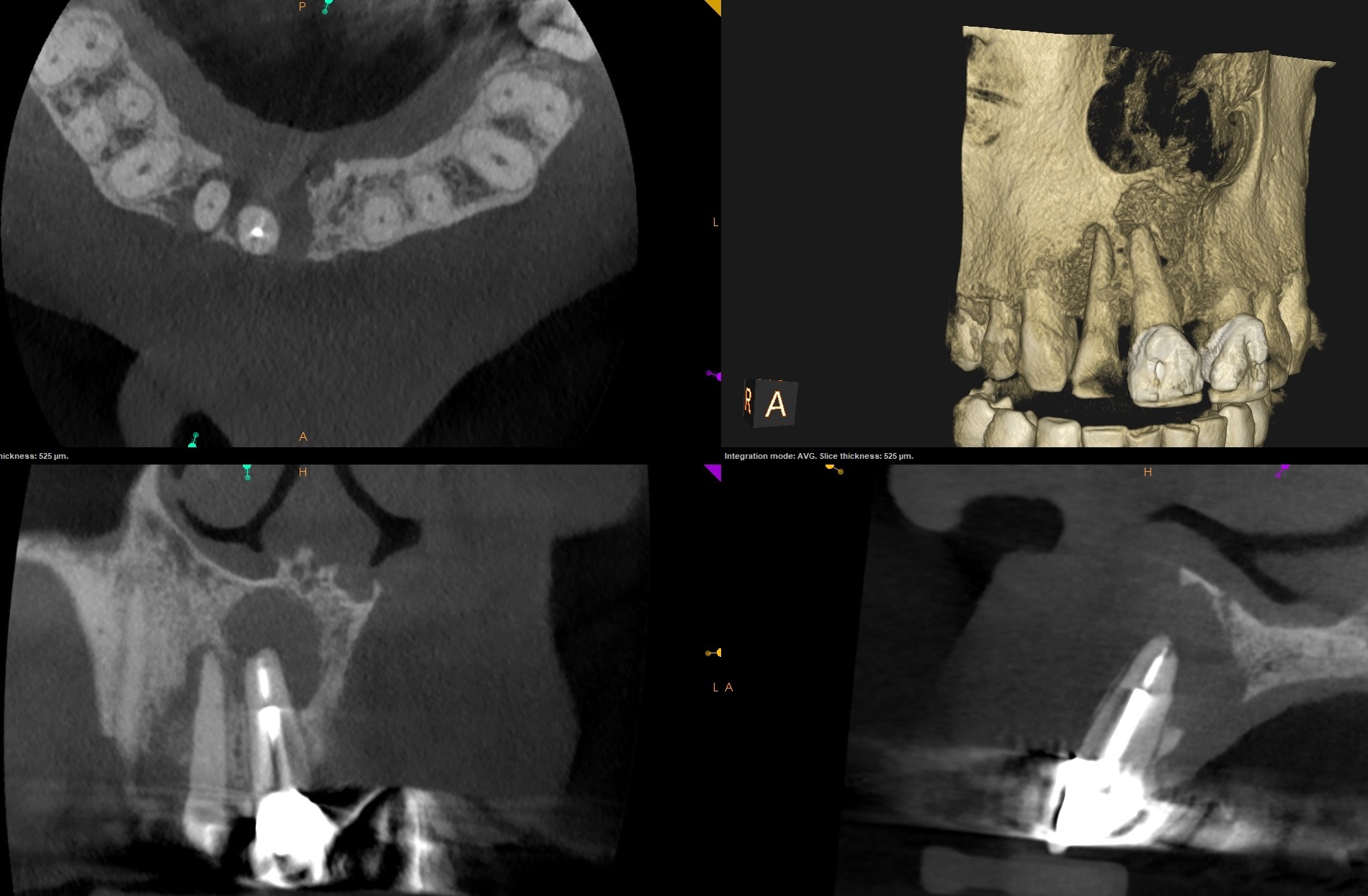
Radiographic evaluation: Periapical radiographs of the maxillary anterior teeth show existing PFM crowns on teeth #8 and #9 with previous root canal therapy of tooth of #8 with a large post. The obturation material is lacking in density in the apical portion of #8. Both #7 and #8 lack a continuous lamina dura and a large periapical radiolucency is present compassing both roots. The severe lack of density within the radiolucency indicates a through-and-through lesion.
A limited FOV CBCT was exposed revealing an area of low density (14x12x10mm in dimension) encompassing the root apices of #7 and #8. Significant erosion of the buccal and palatal cortical plates is evident. The alveolar bone around #7 and #8 is intact circumferentially.
Clinical evaluation: Probing depths 2-3mm across all maxillary anterior teeth. None are tender to percussion or palpation. Tooth #7 responded positively to cold testing.
Tooth #7 has class 1 mobility and #8 has class 2 mobility. A buccal sinus tract is present in the attached gingiva above #7. The #8 and #9 PFM crowns are intact with clinically sealed margins.
Diagnosis:
Tooth #7 normal pulp with asymptomatic apical periodontitis
Tooth #8 previously treated with a chronic apical abscess.
Stay tuned! We'll reveal the actual treatment rendered, and the poll results, in a future edition of The Paper Point!
Dr. Adam Gluskin is a member of the AAE's Resident and New Practitioner Committee.
