President’s Message: Commentary on the 2015 CBCT Position Statement
By Terryl A. Propper, D.D.S., M.S.

The use of cone beam computed tomography seems to be a hotly discussed issue in endodontics. Some clinicians believe that CBCT is a superior diagnostic tool that should be utilized as much as possible, while others insist that two-dimensional radiographs are the standard and continue to be adequate. Though the debate is ongoing, with staunch supporters on each side, it tends to oversimplify the issue. The question should really be focused on the circumstances in which the use of CBCT benefits the patient.
Recently, the AAE Board of Directors reviewed and approved a revised Joint Position Statement from the AAE and the American Academy of Oral and Maxillofacial Radiology on the use of limited field of view cone beam computed tomography in endodontics. The original joint statement on CBCT was issued in 2010, and AAE policy requires that all position statements be reviewed every five years and either revised, reaffirmed or rescinded. The 2015 position statement was drafted by a special joint committee of leading experts in the area of CBCT. Each organization appointed four representatives. Dr. Mohamed I. Fayad of the University of Illinois at Chicago, appointed by the AAE, and Dr. Madhu K. Nair of the University of Florida, appointed by the AAOMR, served as co-chairs of the committee. AAE Members Drs. Craig S. Hirschberg, Martin D. Levin and Richard A. Rubinstein also served on the committee, along with Drs. Sevin Barghan, Erika Benavides and Axel Ruprecht from the AAOMR. There was no input or involvement by outside or corporate entities.
Specifically, the committee was charged with "identifying clinical situations in which the use of CBCT is especially valuable for endodontists." The recommendations in the new statement are supported by the most current scientific literature and based on the principles of ALARA — keeping patient radiation doses "as low as reasonably attainable."
The CBCT statement is not about "cookbook endodontics." It is an educational resource. It is clear that magnification and radiographic imaging are integral to the performance of modern endodontics. Advancements in these areas have helped us save more teeth as well as identify when a tooth cannot be saved. The ultimate decision to use a particular diagnostic tool or perform a specific procedure must be made by the clinician in light of all the circumstances, including the clinician's training and experience, the condition and preferences of the patient, and available resources.
Endodontists continue to have excellent results with two-dimensional radiography. The AAE and AAOMR agree that CBCT should not be used routinely for endodontic diagnosis or screening purposes in the absence of clinical signs or symptoms. However, CBCT does have a place in endodontic diagnosis, when dealing with more complex cases. Our goal is to help AAE members determine where it fits for them.
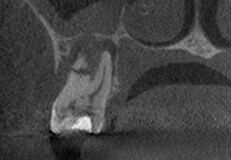
Preoperative 2-D X-ray (left), compared to axial 3-D (center) and sagittal 3-D (right) renderings. The 3-D renderings were used to determine the presence and location of missed lingual canals prior to retreatment. Photos courtesy of Dr. Mohamed Fayad.
Using CBCT in diagnosis and treatment does not require owning a CBCT. It is common for endodontists to "refer" cases that they think will benefit from a CBCT to a provider who owns a limited field of view CBCT and is experienced in taking the image and interpreting the results.
Another question that arises when discussing CBCT is, "Does insurance cover this?" While we do not have a definitive answer to this yet, the AAE is working diligently to educate the major insurers and advocate for coverage when it is appropriate. In 2014, I had the privilege of representing the AAE at our biennial meeting with dental directors for large dental insurance plans. We discussed CBCT and endodontics, and the fact that plans are reluctant to cover CBCT for endodontic claims. While we recognize that the revised statement, which the AAE has shared with this group, is not a "magic bullet" that will convince insurers to reimburse CBCT, we also know that we are not going to move the needle without clinical rationales supported by scientific literature.
In May 2015, Immediate Past President Dr. Robert S. Roda, along with Drs. Kenneth B. Wiltbank and Ali Behnia, had the opportunity to advocate for the clinical benefits of CBCT scans with dental insurers again when they attended the American Association of Dental Consultants Workshop. At the workshop, Dr. Roda gave a presentation illustrating clinical cases and indications for clinical use of the limited FOV CBCT as it applies to everyday endodontic practice. He also emphasized that paying for a diagnostic CBCT scan, when indicated, could prevent endodontists from performing a procedure that would have a poor prognosis. The dental directors were impressed with the presentation, and they felt that it gave them insight into the judicious use of CBCT in clinical practice.
Then perhaps the real question is, "Does having the ability to see a tooth in three dimensions alter the diagnosis?" Based on my experience, I'd have to say yes. I practice with seven other endodontists and we have been referring all of our CBCTs to a periodontist when we felt we needed to look at a tooth in three dimensions. After much discussion and trepidation (mainly over cost), we agreed that our lack of a limited FOV CBCT was inhibiting our ability to practice endodontics to the best of our abilities. A limited FOV CBCT would allow us to better see resorptive defects, to know with assuredness that we have not missed a canal, to diagnose teeth that should not be retreated, to better determine bone loss, and to help identify landmarks during apical surgery. As a friend and colleague said to me, "Terryl, when you don't have a CBCT in your office, you don't realize how much time and effort it can save you during a treatment procedure, looking for a canal or determining why a previous treatment failed. You just don't know what you don't know!"
Preoperative 2-D X-ray (left), compared to the 3-D sagittal view (center) and coronal view (right) of a root fracture. In this case, the distal root fracture was not visible or detected on the digital radiograph. Photos courtesy of Dr. Mohamed Fayad.
The doctors in my practice all agreed that the AAE/AAOMR position statement, combined with our experience seeing clinical cases in everyday practice that could benefit from 3-D images, justified the purchase of a CBCT. In addition, an increasing number of our referring dentists now own CBCT themselves — clearly, the time has come to enhance our own ability to see in three dimensions. We placed an order for three limited FOV cone beams, one for each of our three locations.
I know that my experience may not apply to everyone, and that the revised position statement will not definitively end the CBCT debate. It is important, however, to consider CBCT's effect on our clinical abilities, patient care and unique value as specialists. As technology advances, so does our specialty. The next technological innovation is on the horizon and the AAE and academic and clinical endodontists will continue to evaluate what is best for our specialty, based on the most advanced scientific evidence and research.
View and download the revised AAE/AAOMR Joint Position Statement at www.aae.org/guidelines.
Additional CBCT Resources
The following sessions from AAE15 are now available to subscribers for online CE credit through the AAE Live Learning Center:
- 3-D Imaging and Surgery — Mohamed I. Fayad, D.D.S., M.S., Ph.D.
- Advanced Uses of CBCT in Endodontics — Evan R. Chugerman, D.M.D., and Michael J. Feldman, D.M.D.
- Assessing Endodontic Outcomes With CBCT — Jeffery B. Price, D.D.S., M.S.
- Endodontics in the 21st Century: What Is the Fourth Dimension? — Mohamed I. Fayad, D.D.S., M.S., Ph.D.
- Impact of CBCT in Clinical Endodontic Practice: Advances, Limitations and Medical Legal Considerations — Bernard Friedland, B.Ch.D., M.Sc., J.D.