The American Association of Endodontists (AAE) proudly led a record-breaking grassroots advocacy effort—the largest in its history—to protect the financial foundation of endodontic practices nationwide. Demonstrating unwavering conviction, AAE leadership mobilized with urgency and clarity as President Dr. Steven Katz issued a powerful call to action on May 22, urging members across the country to contact their U.S. Senators. AAE members responded in force, uniting behind the Association’s leadership to oppose a harmful provision in the House-passed budget bill that would have eliminated key tax protections for dental professionals and imposed significant financial burdens on specialty practices.
AAE took swift and decisive action against the proposed elimination of the Pass-Through Entity Tax (PTET) deduction. This measure would have dramatically increased the tax burden on countless dental practices, including many owned and operated by AAE members. The provision targeted pass-through entities such as S-corporations and partnerships, which currently benefit from the ability to deduct state and local taxes (SALT) on their federal tax returns. The proposed change would have stripped that deduction, leading to significant tax increases at a time when practices are already grappling with rising operational costs and economic uncertainty.
AAE made it clear that for endodontists in private practice, the financial impact of such a policy shift would be unsustainable. With inflation, staffing pressures, and supply chain challenges already straining resources, additional tax liabilities could have forced difficult decisions about access, growth, and even continuity of care. The Association stood firmly with its members, amplifying their voices in Washington to protect their ability to serve patients and communities with excellence. In addition, AAE joined fellow dental organizations in signing the Organized Dentistry Coalition (ODC) letter to Congress, reinforcing a unified message in defense of PTET and fair tax policy for dental professionals.
AAE is pleased to announce that its advocacy efforts have secured a significant victory. The Senate version of H.R. 1, the exact legislative vehicle that previously threatened the PTET deduction—does not include any restrictions on this vital tax relief. This means that current tax law remains unchanged, preserving the full SALT deduction for pass-through entities, including dental entities, and safeguarding members from a potential 1.5% to 5% increase in their federal tax bills.
The AAE views this development as the best possible outcome for both the endodontic community and the broader dental profession. It not only ensures critical financial stability for specialty practices but also serves as a strong testament to the strength and unity of our grassroots movement. Hundreds of AAE members took the time to write to their respective Senators, demonstrating how collective action, fueled by member dedication, can effectively influence federal policy and safeguard the future of our profession.
AAE celebrates this win, but the work is not over. Final passage of H.R. 1 in both chambers of Congress must still occur without any modifications to the PTET provision. The Association remains vigilant and fully committed to protecting this hard-fought progress, ensuring that the interests of endodontists stay front and center in national policy decisions.
Together, we are demonstrating the possibilities when advocacy aligns with unity—and how the collective voice of the endodontic profession can influence the laws that impact specialty practice.
We are excited to share a byline article from AAE President Dr. Steven J. Katz on the popular website KevinMD.com.
In this article, Dr. Katz tackles the timely topic of water fluoridation — explaining why removing fluoride from the water is a public health disaster.
Founded in 2004 by Kevin Pho, MD, KevinMD is the web’s leading platform where physicians, advanced practitioners, nurses, medical students, and patients share their insights and stories. He has a broad and influential reach: 274k+ followers on LinkedIn, 153k+ on Twitter, and more than 150k newsletter subscribers. The site receives approximately 188k visits each month.
It’s just the latest example of endodontists sharing our wisdom and broadening our reach!
Call to Order
President Natasha M. Flake called the 2025 General Assembly of the American Association of Endodontists to order at 8:50 a.m. on April 4, 2025, at the Hynes Convention Center in Boston, Massachusetts. A quorum of voting members was in attendance. President Flake instructed the assembly on voting procedures for the meeting.
Standing Rules for the General Assembly were published online with the General Assembly meeting materials and were reviewed at the outset of the meeting.
President Flake appointed Dr. Mark Desrosiers to serve as parliamentarian for the 2025 General Assembly.
Approval of Minutes
President Flake called for approval of the minutes of the 2024 General Assembly as published in the Communiqué.
GA-1 Moved: That the 2024 General Assembly Minutes be approved as published.
Motion Carried.
Report of the Constitution and Bylaws Committee
Constitution and Bylaws Committee Chair Dr. Craig S. Hirschberg presented two proposed amendments to the Constitution, published in the January 2025 issue of the Communiqué.
The first proposed amendment enables the Board to remove a Director with a 3/4 vote in the case that the Board concludes that continued service on the Board would be contrary to the best interest of the Association, rather than only allowing the Board to remove a Director in case of an emergency. The proposed amendment retains the General Assembly’s right to remove a board member with a 2/3 vote.
GA-2 Moved: that the proposed amendment to Article V, Section 5 of the AAE Constitution relating to the process to remove a Board member be approved.
Motion Carried.
The second proposed amendment reflects that only members in good standing of the AAE (rather than of affiliate associations) are eligible to serve on District Caucus Nominating Committees.
GA-3 Moved: that the proposed amendment to Article X, Section 4 of the AAE Constitution, relating to service on District Caucus Nominating Committees, be approved.
Motion Carried.
Both motions amending the Constitution passed with the required ¾ affirmative vote.
Reports of Officers
Written reports from the AAE President, Secretary, and Treasurer were made available to members online prior to the meeting.
Treasurer’s Report
AAE Treasurer, Dr. Elizabeth Shin Perry, reported that for the fiscal year that ended on June 30, 2024, the AAE had an operating surplus after investment earnings of $299,000. Strategic initiative spending totaled $583,000 resulting in a bottom-line deficit of ($284,000). Strategic initiatives focus on the public, the profession, and membership.
In addition, AAE received a clean audit from its independent auditors, indicating that financial operations not only comply with Generally Accepted Accounting Principles, but also that the association is financially sound and that the Board of Directors has operated responsibly and in the best interest of the AAE and its membership.
Dr. Perry reviewed AAE Operating Revenues, Expenses, and Operating Surplus, Strategic Initiatives, and Total Surplus/Deficit for the years ending June 2022 through June 2024.
For Fiscal year 2025, an operating deficit of ($332,000) and a total deficit of ($998,000) are forecasted. The projected deficit also includes expenses related to strategic initiatives. These final results are lower than the prior year due to the impact of inflation on expenses, conservative forecasts for annual meeting and a changing vendor marketplace.
The AAE Investment balance at June 30, 2024 equaled $13.4 million and was 96% of the 2024 annual expenses. AAE is currently in a strong financial position with investments equal to over 90% of one year’s expenses.
Dr. Perry reported that the Board of Directors approved a Fiscal Year 26 budget projecting revenue of $12,751,000, expenses of $13,654,000, investment earnings of $376,00 with an operating deficit of ($527,000). This deficit is greater than the current year, as we expect AAE to minimize expenses and expand revenues to reduce this conservative estimate.
The board is advancing the strategic plan which focuses on expanding the public’s awareness of endodontics, developing knowledge to advance the specialty, advocating for quality endodontic care, and supporting members to advance the specialty. The board approved additional funding for the strategic initiatives in the amount of $561,000. This will be funded in Fiscal Year Budget 26 through the use of reserve funds. This strategic spending level is similar to prior years, and AAE’s strong financial position allows the organization the opportunity to invest in new initiatives to strengthen the profession.
Journal of Endodontics Report
JOE Editor-in-Chief, Dr. Kenneth M. Hargreaves, reported continued advances in the Journal of Endodontics.
JOE continues to attract noteworthy papers from researchers and clinicians around the world. There has been a 266% increase in the number of new manuscripts submitted to the JOE from 2003-2024.
This increase in submissions consisted of many manuscripts of good quality. In addition to the 1,131 new manuscripts submitted in 2024, an additional 253 revised manuscripts were submitted in response to a prior review. Thus, the Editorial Board reviewed a total of 1,384 manuscripts submitted in 2024, which equates to about 3.8 papers submitted every day throughout the year.
With more than 382 endodontists and scientists from more than 25 countries currently serving as members of the Scientific Advisory Board (SAB), the JOE represents a substantial commitment to excellence by AAE members and endodontists around the world.
The JOE has developed an outstanding Impact Factor over the last two decades. Other measures are also quite strong: in 2023, the JOE generated twice as many citations and published more papers than the IEJ.
The JOE Awards were presented at the JOE Award and Scientific Advisory Board Reception recognizing the best articles in the categories of Basic Research: Biology, Basic Research: Technology, Case Reports and Clinical Techniques, Clinical Research, Regenerative Endodontics, and Systematic and Scoping Reviews. In addition, 6 papers published in 2024 received Honorable Mentions. Nominations for next year’s awards will open in the fall and members are encouraged to submit nominations to recognize their peers who are shaping the future of the specialty.
Dr. Hargreaves closed by celebrating a significant milestone – the 50th anniversary of the Journal of Endodontics.
Foundation for Endodontics
Foundation for Endodontics President Dr. Patricia Tordik reported that the Foundation continues to support the specialty through on research, education, and access to care. In 2024, the Foundation supported endodontics with over $1.4 million in grants.
Dr. Tordik reviewed new programs launched by the Foundation in 2024:
- The Foundation & Dentsply Sirona Freedom Scholarship provided $50,000 for tuition and fees for three endodontic residents.
- With a new partner supported by the Sandals Foundation, the International Access to Care Program sent four endodontic residents and two endodontist mentors to the Caribbean to care for an underserved population.
- The Part-time Educator Development Grant provided nearly $15,000 to fourteen endodontic educators from eleven programs supporting their continuing education.
In 2025, partnering with Cornerstone Dental Specialties, the Foundation will recognize newly boarded endodontists with a $500 gift as a token of appreciation for their commitment to the specialty.
The Endodontic Educator Fellowship Award helps to ensure that endodontics at every level is being taught by skilled endodontists. Dr. Xiaofei Zhu, assistant professor and research director of endodontics at Boston University, was recognized as the 2024 Endodontic Educator Fellow.
2024 was a rewarding year for the Domestic Access to Care program; five projects across the U.S. were funded, providing access to endodontic care to a variety of vulnerable populations, including the homeless and others living below the poverty level. The Foundation is appreciative of this program’s industry supporter, Specialized Dental Partners, for their commitment to sustain this program through 2025.
Dr. Tordik recognized and thanked the Foundation’s first time and repeat contributions from industry partners and encouraged members to become Foundation donors.
Several grassroots efforts raised funds in honor of 2025 AAE award winners. Dr. Tordik noted that the donations in honor of Dr. Kenneth Hargreaves will allow the Foundation to award a Full-Time Educator Development grant in his name, every year in perpetuity. Recipients of the Foundation’s named educator development grants were recognized.
American Board of Endodontics Report
ABE President Dr. Avina Paranjpe presented the report of the American Board of Endodontics. Dr. Paranjpe reported in 2024, the ABE examined 201 Oral Exam candidates, reviewed 147 Case History Portfolios, and administered the Written Exam to 232 examinees through the Pearson Vue testing centers. Dr. Paranjpe congratulated the 116 new Diplomates, noting that this is among the highest number of Diplomates to be honored at an Annual Meeting.
The ABE Board elected to administer the case history exam once per year starting in 2024, and evaluated all the portfolios submitted during the first annual exam. The Oral Exams continue to be administered twice a year in March and October, and the Written Exam is given annually over one day in May.
Dr. Paranjpe expressed the ABE’s thanks to dedicated past Directors who continue to volunteer and serve as examiners for both the Case History and Oral Exams.
110 Diplomates completed their Recertification requirement in 2024. The ABE continues to monitor the requirements set forth by the National Commission on Recognition of Dental Specialties and Certifying Boards (NCRDSCB) so that all aspects of our processes comply, including requirements for the Recertification of Board-certified endodontists.
ABE staff were thanked for their contributions to the ABE’s success. Dr. Paranjpe encouraged interested members to nominate themselves for Board service and encouraged members to seek Board Certification.
Presentation of ABE Nominees
ABE President Avina Paranjpe presented the following slate of nominees for ABE Directors:
Joseph M. Dutner, Director, Second Term
Garry L. Myers, Director, Second Term
Renato M. Silva, Director, Second Term
Amir Azarpazhooh, New Director
Terry D. Webb, New Director
Dr. Paranjpe also announced the ABE’s officers for 2025-2026:
Meetu R. Kohli, President
Joseph M. Dutner, Vice President
Garry L. Myers, Secretary
Scott L. Doyle, Treasurer
Nominating Committee Report
AAE Nominating Committee Chair, Dr. Alan S. Law, presented the slate of nominees for AAE officers and Foundation for Endodontics Trustees:
American Association of Endodontists
President: Steven J. Katz
President-elect: W. Craig Noblett
Vice President: Elizabeth Shin Perry
Secretary: Mark B. Desrosiers
Treasurer: Bradley H. Gettleman
Immediate Past President: Natasha M. Flake
Foundation for Endodontics Trustees
Dustin S. Reynolds, Trustee
Rene Chu, Trustee
Jack Burlison, Public Sector Trustee
Amy Warren-Kimbro, Public Sector Trustee
Judith Forsythe, Public Sector Trustee
Dr. Law also announced the 2025-2026 officers for the Foundation for Endodontics which have been elected by the Foundation’s Board of Trustees:
President: Patricia Tordik
President-elect: Clara M. Spatafore
Treasurer: Robert S. Roda
Secretary: Bruce C. Justman
District Director Nominees
President Natasha M. Flake presented the slate of nominees for District Director positions:
District II: Carla Y. Falcon
District IV: John M. Nusstein
District V: Poorya Jalali
District VI: Katherine Divine
Election of Board Members
There being no other nominees, the slate of nominees for Officers and Directors of the AAE, Directors of the American Board of Endodontics, and Trustees of the Foundation for Endodontics were elected for terms beginning in 2025.
New AAE officers and district directors, ABE directors, and AAE Foundation trustees took an oath to abide by the Constitution and Bylaws of the American Association of Endodontists and the Bylaws of the respective organizations to which they have been elected, and to discharge their duties and responsibilities to the best of their abilities.
Outgoing President’s Remarks
Immediate Past President Natasha M. Flake thanked the Assembly for the opportunity to serve as AAE President. Dr. Flake emphasized a year of collaboration, advocacy, and strategic progress. Key achievements include defeating restrictive legislation, enhancing public awareness, and strengthening inter-organizational partnerships to improve patient care.
Incoming President’s Remarks
Dr. Steven Katz opened his remarks by thanking the Nominating Committee, Board of Directors, Executive Committee, and AAE staff for their confidence and support. He reflected on his journey to leadership and years of service within the AAE, highlighting his involvement in AAE’s public and patient education campaigns. Dr. Katz emphasized the strength of the AAE as a growing specialty organization with over 8,100 members and an 82% domestic membership rate, noting that public awareness and patient demand for endodontic care continue to rise.
He addressed several critical challenges facing the specialty, including a nationwide shortage of endodontic educators, legislative threats to specialty recognition, and broader federal issues impacting dental education and research funding. Dr. Katz concluded by encouraging members to engage in AAE programs, participate in education and advocacy, pursue board certification, and support the Foundation, emphasizing that collective involvement is key to preserving the excellence and future of the profession.
New Business
No new business was submitted for consideration by the Assembly.
Adjournment
There being no further business, the 2025 Meeting of the AAE General Assembly was adjourned at 9:50 a.m.
The AAE is thrilled to announce our 10 Save Your Tooth Month Social Media Endofluencers of 2025! These Instagram accounts went above and beyond this past May in celebration of #SYTM2025. They touted our specialty via creative posts, reels, giveaways and more, and emphasized the importance of saving one's natural teeth.
A gracious honorable mention goes out to everyone who posted about SYTM or changed their profile photo to include our special SYTM frame. Our reach gets a little wider every year, and we couldn't do it without each of you spreading the word.
Learn more about our SYTM Endofluencers below! Give them a follow and get inspired by their social savviness, all year-round.
Edgewater Endodontics
(@edgewater_endodontics)
Brains behind our social media:
Dr. Rob Heydrich and the entire Edgewater team
Why we decided to be active on social media during SYTM / the effect it had on our team:
Our practice has been active on social media for several years, but Save Your Tooth Month brings a special energy to our content. It’s that time of year when the endodontic community comes together to champion the importance of saving natural teeth. The enthusiasm is truly next level.
Our posting process:
The original plan was simply to create some content for Save Your Tooth Month (SYTM). The process is dynamic and driven by inspiration—we might be sparked by a trending topic, something we see or hear, or anything that reminds us of teeth or endodontics. From there, we use the Canva app to bring the idea to life as a meme or video, and the concept evolves organically. The only limit is your imagination.
Advice for endos trying to up their social game, our favorite platform, and how we find time to post:
Just go for it—find something interesting, inspiring, or funny related to endodontics or your practice, and turn it into a post.
Instagram is our preferred platform because it’s quick and easy to use. Creating content doesn’t take much time, but finding the time can be a challenge. If you're short on time, consider outsourcing the task.
Our favorite SYTM moment:
The "How to Spot Misinformation" series was phenomenal and incredibly timely. Over the past year, we’ve noticed several so-called online "health experts”—unfortunately, including some dentists—spreading misinformation about long-debunked health concerns related to root canal treatments. It was great to see the AAE release content that directly challenges this misinformation. The videos were exceptionally well produced and will have a lasting impact well beyond Save Your Tooth Month 2025.
Evolution Endodontics & Periodontics
(@evolutionendodontics)
Brains behind our social media:
Adriel Shulz (The Social Molar), Drs. Shaun Soucie, Arthur Yagudayev, and Sarah Lowder
Why we decided to be active on social media during SYTM / the effect it had on our team:
Our office is deeply committed to treating patients with compassion and care. We continuously integrate the latest advancements in technology to not only enhance patient outcomes, but to uphold the highest standards within our specialty.
We have a strong commitment to excellence and a mindset of continual growth. Becoming more active on social media and promoting endodontics felt like a natural extension of that mission and Save Your Tooth Month provided the perfect opportunity to showcase the work we do and the heart behind it.
Our posting process:
We did plan out our content in advance! We recently began working with a social media company that specializes in endodontics, and they’ve partnered closely with our team to create content that’s both fun and educational. It’s been a great way to stay consistent and highlight the value of our specialty in a creative and engaging way.
Advice for endos trying to up their social game, our favorite platform, and how we find time to post:
Start small and stay consistent. In today’s digital world, having an online presence is essential—patients and referring offices are turning to social media to learn more about who you are and what you do. You don’t need to overcomplicate it highlight what makes your practice special, educate patients, and don’t be afraid to show your team’s personality. Involving your team is key, and if content creation isn’t something they can commit to consistently, there are resources and companies that can help. The most important thing is to just start.
We love Instagram! It’s a great visual platform that allows us to connect with both patients and referring offices. The mix of Reels, Stories, and posts gives us creative flexibility and helps us keep things both educational and fun.
Planning ahead has been a game-changer. We recently started working with a social media company that specializes in endodontics, and they’ve helped our team plan, and produce content that fits our schedule. We also make it a team effort when everyone knows what’s needed and we carve out time in advance, even just a few minutes here and there can go a long way.
Our favorite SYTM moment:
We really enjoyed seeing all the creative content shared by other practices and staying involved with the AAE community. It was such a great opportunity to come together as a specialty and highlight the importance of saving natural teeth. The energy and collaboration made it both fun and meaningful for our whole team.

Root Canal Specialty Associates
(@rootcanaldocs)
Brains behind our social media:
Michele Brautnick, Dr. Martha Zinderman (President) and Kimberly Middlekauff (Director of Operations)
Why we decided to be active on social media during SYTM / the effect it had on our team:
Participating in Save Your Tooth Month is an annual marketing effort for us. We often create content designed to change the perception of root canals to help patients understand why saving their natural teeth, if possible, is always the best option. Emphasizing this message collectively with other endodontists and the AAE makes good sense for our brand.
Our posting process:
We plan all of our social content, especially our SYTM plans. Being prepared ensures consistency in terms of messaging and the frequency of our posts. It also forces us to serve up a good mix of content designed to educate, entertain, and inspire.
Advice for endos trying to up their social game, our favorite platform, and how we find time to post:
We would encourage other endodontists to leverage social media to inform patients about the safety and effectiveness of root canals. There is still so much misinformation out there about root canal treatment. Together we can change the perception and help alleviate patient anxiety.
Our favorite SYTM moment:
In celebration of summer and the sports injuries that can come along with it, we used this opportunity to remind patients and referrers that teeth can take hits, just like the rest of the body. If dental trauma occurs, endodontists can help.
St. Petersburg Endodontics
(@stpeteendo)
Brains behind our social media:
Ashley George (content creator) and Missy Gater (office manager/marketing oversight)
Why we decided to be active on social media during SYTM / the effect it had on our team:
Preserving natural teeth is at the forefront of what we do, so participating in Save Your Tooth Month was a natural fit. We believe in the power of education, prevention, and compassionate endodontic care, so this campaign gave us an opportunity to amplify that message beyond the office. Through outreach, social media, and conversations with patients, we aimed to highlight the value of endodontics in a way that was engaging and approachable.
Our posting process:
We planned our content at least a week in advance— sometimes more if we had concepts that could be quickly executed. We tried to incorporate a mix of reels, carousel posts, and eye-catching photos/graphics while showcasing different themes, like endodontic education, highlighting Dr. Hedrick, and overall, the importance of saving natural teeth.
Advice for endos trying to up their social game, our favorite platform, and how we find time to post:
Start by showing up consistently and authentically. You don’t need to be flashy or have “perfect” content. Share what you know, what you're learning, or even just what excites you about endodontics!
We primarily use Facebook and Instagram, aiming to post (at least) a few times each week. We often draft captions or outline ideas before we even have the final photo or reel. This approach helps us stay consistent and efficient once the right visuals are ready.
Our favorite SYTM moment:
We enjoyed posting about the importance of saving teeth, featuring our doctor and staff, and showcasing some of our office’s technology. While there wasn't one standout moment, it was rewarding to contribute meaningful content throughout the month.

Afton Endodontics
(@aftonendodontics)
Brains behind our social media:
Katelyn Rios (Marketing & Social Media Manager), Drs. Kathryn Watts, Zak James, and Gregory Gell
Why we decided to be active on social media during SYTM / the effect it had on our team:
Save Your Tooth Month is the perfect opportunity to educate the public about the value of root canals and the role endodontists play in saving natural teeth. At Afton Endodontics, we’ve always believed in using social media as a tool to connect, inform, and make dentistry feel less intimidating. Being active during SYTM let us show off not just our clinical expertise, but our personality and values as a team. This year, we partnered with 12 local businesses to run a series of community giveaways throughout the month. It was such a fun project to work on—not only did it allow us to support and spotlight other small businesses, but it also helped us reach a much wider audience than we could have alone.
Our posting process:
This year was a little different for us! We had a general plan going into Save Your Tooth Month, with a strong focus on community giveaways and educational content. We outlined what we wanted to cover each week and made sure we featured both our clinical and front office teams. Most of the content was created and posted in real time, depending on what we had going on in the office or with our giveaway partners. It was a flexible approach, but still intentional—we knew what we wanted to highlight, and we made it happen.
Advice for endos trying to up their social game, our favorite platform, and how we find time to post:
Start small and be authentic. Patients and referring offices want to know you, not just textbook dentistry. Share your team, your values, and what makes your practice unique. Instagram is our favorite platform—it’s visual, versatile, and works well for both educational and fun content. As for time: we treat content creation like any other marketing task. We block off time for photos/videos, and we repurpose content across platforms to get the most out of each idea. Planning ahead really is the game-changer to stay consistently.
Our favorite SYTM moment:
Definitely the giveaways. We partnered with 12 local businesses, and getting to visit them in person, collaborate, and create content together was such a fun shift from how we’ve done SYTM in the past. It gave us the chance to connect with new people in our community and expand our reach by tapping into the networks of these amazing local brands.
It also got the staff at our referring offices involved in a new way—especially the front desk teams and dental assistants, who are often the ones actually making referral decisions. That kind of engagement is exactly what we hope for. Stepping outside the box this year really paid off, and we were excited to do something that brought value to both our audience and our community.

Advanced Endodontic Care
(@advancedendodonticcare)
Brains behind our social media:
Adriel Schulz, Drs. Rolf M. W. Wuerch, Stephen W. Hansen, and Jeremiah J. Hawkins
Why we decided to be active on social media during SYTM / the effect it had on our team:
We love using Save Your Tooth Month as an opportunity to spotlight endodontics! Our team has always taken an active role in our social media, but this year, we took it a step further by involving our community. We filmed content while engaging with local businesses and referring offices, sharing more about root canals and what makes our specialty so important. It was a meaningful way to connect and educate.
Our posting process:
This year, our team did something a little different by stepping outside the office and into our community. Leading up to the month, we thoughtfully planned which local offices and businesses we wanted to connect with and reached out ahead of time to coordinate.
We also brainstormed content ideas earlier in the year so we could stay organized and intentional with our posts. With a goal of sharing a couple of times a week, we pre-filmed some videos to fit around our schedule and make sure our content was ready to go.
We chose proven posting times in each platform to have the greatest reach for our audience, since we do promote on 3 different social media platforms.
Advice for endos trying to up their social game, our favorite platform, and how we find time to post:
You can start simple the key is consistency. You don’t need to reinvent the wheel; just share what makes your practice special. Patient education, behind-the-scenes moments, and team highlights go a long way in building trust and visibility. Don’t be afraid to show your personality. You’re not just speaking to referring offices you’re also showcasing your role in the community. Authenticity always resonates, and it’s a great way to show that root canals don’t need to be feared.
If possible, delegate or collaborate with a team member who enjoys content creation. This doesn’t have to fall on the doctor your team is often more than capable. Sometimes, they just need the green light to take the lead, and you to set clear expectations of what you would like.
Instagram is our favorite! It’s visual, and easy to use. We also utilize TikTok and Facebook, they all have different benefits and reach a variety of people. Using a variety allows us to connect with both patients and referring offices in a fun and interactive way. Between posts, Reels, and Stories, there’s a lot of creative freedom to showcase endodontics in a more approachable light.
Planning ahead is key! We usually brainstorm ideas in advance, and getting the team excited makes a big difference they’re often eager to create content. Of course, patient care is always the top priority, so we schedule specific times during the day or week to take just a few minutes to film. When everyone is prepared and knows what’s needed ahead of time, the process becomes simple and efficient. If this isn’t something you can take on in office, there are companies that specialize in social media for dental practices and they can be a great resource to help you stay consistent and on-brand.
Our favorite SYTM moment:
We definitely loved all of it - creating our dental dam video, connecting with our community (some even invited us to come film with them!), and of course, seeing all the great content shared by other offices. It was such a fun and rewarding way to celebrate Save Your Tooth Month together!
Meares Becker Endodontics
(@mearesbeckerendodontics)
Brains behind our social media:
Tracy Meares, Drs. William Anthony Meares and Adam Becker
Why we decided to be active on social media during SYTM / the effect it had on our team:
We are trying to utilize all marketing avenues. I am using our Facebook and Instagram more as an alternative "landing page" to complement our website. Since social media is more popular than websites, our goal was to present some of the same information from our website but in a different way. To appeal to people who might prefer using these platforms instead of a traditional website.
Our posting process:
My goal was to have a few posts with the SYTM logo and highlight some of our 5 star google reviews. In general, I am trying to go for a modern esthetic. I use Canva to make the posts and try them out on an offline grid I made to see how they will look on my profile. I am trying to mix up informational posts and patient review posts. Slowly I will try to start making posts geared toward referring dentists, but slowly. My goal is to have a mixed appeal to dentists and patients. I use AI platforms to help me with the text that I will tweak before posting.
Advice for endos trying to up their social game, our favorite platform, and how we find time to post:
Instagram is my favorite and is very easy to use. I do not like Facebook but I post there just to have a presence on that space.
I would tell an endodontist to hire someone to do it or if there is someone on staff that has that skill set to get them to help. But I would caution to oversee what they are posting if you go that route, for information accuracy.
Once you have some color schemes and fonts you like it becomes easier. And definitely utilize AI to help generate text, this is the biggest time saver.
Also, the AAE toolkit has some great starting points. You can always take an idea from there and tweak it to make it your own style. Or just use what they have to get started.
Our favorite SYTM moment:
It has been fun to see people in Australia like my posts! I liked the post I used at the start of the month, "Know your Teeth, Save your Teeth" - on the second slide I used one of the AAE's videos of the inside of the tooth. I really appreciate this type of content that you produce for the members to use because that is difficult for me to create on my own.
Emirates Facial and Dental Implant Center
(@drcwb_endoqueen)
Brains behind our social media:
I would like to recognise my husband, Christopher Beecher, my ideas guy, #1 supporter and biggest fan. Humbird Media is my social media content producer and poster. Couldn't keep up without them.
Why we decided to be active on social media during SYTM / the effect it had on our team:
I find it to be a fun process to be a part of the Save Your Tooth Month campaign. It pushes me to find more creative ways to bring out how important it is to save one's teeth.
Our posting process:
Pre-planning is essential to ensure I maintain a consistent and purposeful presence online. I start by outlining key messages I want to share—these often reflect both educational content and topics I feel passionate about. I also spend time exploring social media to gather inspiration and stay informed on trending formats or discussions.
From there, I collaborate closely with my husband and social media manager. We schedule brainstorming sessions to develop concepts, followed by filming. Once the footage is captured, my social media manager assembles the content, and I review everything before giving final approval. Once approved, the posts are scheduled for publishing. This process keeps everything streamlined and aligned with my overall vision.
Advice for endos trying to up their social game, our favorite platform, and how we find time to post:
Make the effort—it’s absolutely worth it. Social media is a powerful tool to reach a wide cross-section of people. Some may never step into your office, but they can still gain valuable insights from your content. It’s not just about attracting more patients or referrals—it’s about using our expertise to combat misinformation and make accurate, evidence-based knowledge accessible. If we don’t speak up, others will fill that space with inaccuracies.
At the moment, I post regularly on LinkedIn, Instagram, and Facebook. I haven’t settled on a single favorite yet, but each platform serves a different purpose and audience, so I enjoy exploring what works best.
As for time—let’s be honest, it’s tough. Between family, work, and church, my schedule is full. I’m fortunate to have my husband’s help and also work with a social media management company that assists with content creation and posting. Delegating in this way allows me to stay present in my practice while still building an educational presence online.

CA Root Docs
(@rootdocsendo)
Brains behind our social media:
Loree Tabigne (RDA/Social Media Coordinator), Drs. Scott Cohen, Mark Stevenson, and Florence Au
Why we decided to be active on social media during SYTM / the effect it had on our team:
We chose to be active on social media during Save Your Tooth Month to raise awareness about the importance of preserving natural teeth. Many patients are unaware that extraction isn't the only solution and that root canal treatment is a highly effective option that can save teeth and maintain long-term oral health. By sharing accurate information and educational content, we hope to reduce fear around root canal procedures and help patients make informed decisions. Our goal is to promote healthy smiles through awareness, education, and trust.
Our posting process:
We carefully planned out SYTM content to ensure timely posting that aligns with our office's values and mission. Our goal was to create content that is both informational and educational while also being patient-friendly for those looking to learn more about root canals. We aimed to strike a balance between providing valuable information and incorporating a fun engaging tone across our social media platforms.
Advice for endos trying to up their social game, our favorite platform, and how we find time to post:
Instagram is the preferred platform due to the personal interactions it allows between endodontists, general dentists and patients. It offers a more personable way to connect and engage with others in the dental community. My advice is to plan your content in advance and follow a consistent posting schedule. This helps ensure you stay organized and don't miss important posts or deadlines and to schedule your posts and connect all platforms through Instagram to help with posting.
Our favorite SYTM moment:
One of our favorite social media moments was when Dr. Au’s interview appeared in our feed — and it was reposted by the AAE! It was exciting to see that recognition and to have the opportunity to reach a wider audience through their platform.

Endodontic Associates
(@endoassociates)
Brains behind our social media:
Lynda Davenport, Lindsay Shinn, Drs. Christopher Cain, Mark Freeland, Michael Murray, Clay Sparrow, Phillip Faucette, Annie Jones, John Workman, and Austin Carr
Why we decided to be active on social media during SYTM / the effect it had on our team:
To us, Save Your Tooth Month is a wonderful annual reset that returns us to the heart of the matter- why we do what we do here at Endodontic Associates! There is so much misinformation and fear mongering out there about our corner of the dentistry. It's very important to us that our patients know the facts- what a root canal is (and what it is not), expectations during and after RCT therapy, etc. It's also a great reminder for us as providers and staff about the importance of education and clear communication with patients who put their faith in us for their endodontic care. When patients understand the whole picture, they can actively participate in their own care, leading to better dental health outcomes.
Our posting process:
We did plan our Save Your Tooth Month posts! Our goal was to build on what we shared during SYTM 2024. Last year was our first time participating, and we focused on the basics- definitions and the origins of endodontics, common symptoms, and misconceptions. This year, we went into a little more detail about endodontic procedures as well as what our practice offers specifically. We divided the month into four parts, focusing on one topic each week. For example, we are so proud to offer the Gentle Wave procedure as well as IV sedation to our patients, so each one of those topics had a week-long focus. We also sprinkled in some fun mid-week trivia questions and fun facts to keep engagement up!
Advice for endos trying to up their social game, our favorite platform, and how we find time to post:
To echo our thoughts from last year (because it can't be overstated), it is imperative to use reliable sources for your social media content! You can put your own aesthetic on your posts/stories/reels to reflect the tone and branding of your practice, but your message has to be sound in order to properly educate your community. AAE.com is the wonderful resource to start with! Instagram is our favorite platform to communicate with our patients as well as referring dentists and colleagues. I (Lindsay) feel extremely fortunate that creating content for Endodontic Associates is a part of my job description. It is an honor to represent our practice on social media! For those who do not have a similar position within their practice, apps like Canva are very user-friendly and make creating post and stories quick and easy!
Our favorite SYTM moment:
We really enjoyed seeing all the endodontic practices that added the SYTM frames to their profile pictures- it's a great reminder that we are all a team on a mission to save those teeth! Also, any time a post of ours was shared to AAE's website was such an honor. And of course, learning that we were being recognized as an "Endofluencer" for SYTM 2025 was another favorite moment!

By Drs. Sami Chogle and Pinelopi Pani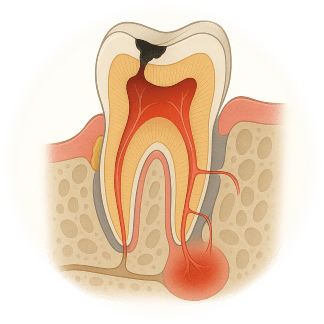
Endodontic-periodontal lesions have complicated etiologies and pathogenic mechanisms, including unique anatomical and microbiological characteristics and contributing factors. In dental practice, few clinical presentations challenge practitioners more than these lesions and the etiological complexity often leads to difficulties in determining tooth prognosis and appropriate treatment. The proximity and interconnection create a bidirectional relationship that allows disease in one tissue to affect the other, resulting in diagnostic gray zones. As specialists we frequently encounter cases that underscore this complexity and demand not only our technical capabilities but also our diagnostic accuracy and interdisciplinary collaboration.
Anatomical Convergence, Clinical Divergence
Dental pulp and periodontium have embryonic, anatomic and functional inter-relationships1. From a biological perspective, the pulp and periodontium function independently, but pathologically, their communication channels (apical foramen, lateral and accessory canals, dentinal tubules) facilitate the spread of bacteria, toxins, and inflammatory mediators. Whether disease initiates in the pulp or the periodontium (figure 1), the resulting lesion can mimic either condition.2 A necrotic pulp can manifest with draining sinus tracts and deep periodontal pockets, imitating periodontal breakdown.3,4,5 Conversely, chronic periodontitis that progresses apically may lead to a cumulative damaging effect to the pulp of more rarely to pulp necrosis.5,6,7,8 Clinical studies have shown that periodontal disease and its treatment rarely results in teeth needing endodontic treatment when the cementum remains intact.9,10 The only exception to this is when the periodontal condition is of such an extent that a pocket reaches the apical foramen. In such advanced periodontal disease, the pulp’s defenses can in some cases be overwhelmed, thus succumbing to infection and ultimately pulp necrosis occurs. The difficulty lies in distinguishing primary disease origin when clinical signs overlap.
Diagnostic Challenges
Misdiagnosis often arises from an overreliance on isolated findings—probing depth, radiographs, or symptoms—without integrating a full diagnostic picture. This may not account for additional findings such as cracks, fractures, resorptive defects or cemental tears. A comprehensive approach including Vitality testing (thermal, electric), Radiographic evaluation with CBCT, tracing of sinus tracts, if present, and comprehensive probing for attachment loss along with mobility assessment could help reduce diagnostic error. A new classification, proposed by the World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions in 201811, focused on the prognosis of involved tooth. The classification is based primarily on the following signs and symptoms of the involved tooth: presence/absence of root damage and anatomic problems; presence/absence of full-mouth periodontitis; and severity and extent of the periodontal defect of the affected tooth, including furcation involvement.
Strategic Sequencing in Therapy
A significant dilemma is not just diagnosis, but treatment sequencing as well. Based on evidence (REF) and clinical observation, we advocate addressing the endodontic component first when the pulp is non-vital. This helps eliminate intraradicular infection, allowing time to observe healing and reevaluate the periodontal status. Periodontal therapy should follow only, if necessary, guided by the healing response after root canal therapy. On the other hand, pulp necrosis from periodontitis is rare; massive bone loss must reach the apex before bacteria threaten the canal.7 Vital pulps tolerate periodontal surgery well with only mild pulpal inflammatory reactions. But more importantly, re-attachment in periodontal therapy outperforms expectations when the pulp remains intact.12 Thus, intervention should be biologically justified—never reflexive.
When Root Damage Changes the Game
Treatment attempts for vertical root fractures remain hopeless, prompting extractions to prevent futile costs. Other failures may result as a consequence of delayed detection and referral, incomplete canal disinfection, ignored mobility, existing root damage (e.g. microfractures, cemental tears) and patient non-compliance. (Fig 1.) By contrast, external cervical resorption (ECR) deserves nuance. Since endodontic obturation alone seldom halts ECR, a combined may be mandatory. And classifying the stage of ECR utilizing a limited-FOV CBCT would influence the endodontic-periodontal surgical intervention prognosis.13
Conclusion
Endodontic and periodontal dilemmas reflect the interconnected nature of dental tissues—and the importance of integrated clinical thinking. As tools evolve and diagnostic precision improves, these challenges will remain part of daily practice. But with thorough evaluation, coordinated care, and respect for biological principles, we can resolve even the most complex cases with confidence.
References
- Mandel E, Machtou P, Torabinejad M. Clinical diagnosis and treatment of endodontic and periodontal lesions. Quintessence Int. 1993;24(2):135–9
- Simon JH, Glick DH, Frank AL. The relationship of endodontic-periodontic lesions. J Periodontol. 1972; 43: 202–208.
- Seltzer S, Bender IB, Ziontz M. The interrelationship of pulp and periodontal disease. Oral Surg Oral Med Oral Pathol. 1963; 16: 1474–1490
- Rubach WC, Mitchell DF. Periodontal disease, accessory canals and pulp pathosis. J Periodontol. 1965; 36: 34–38.
- Langeland K, Rodrigues H, Dowden W. Periodontal disease, bacteria, and pulpal histopathology. Oral Surg Oral Med Oral Pathol. 1974; 37: 257–270.
- Czarnecki RT, Schilder H. A histological evaluation of the human pulp in teeth with varying degrees of periodontal disease. J Endod. 1979;5(8):242–53.
- Zehnder, M. Endodontic infection caused by localized aggressive periodontitis: A case report and bacteriologic evaluation. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontics 2001; 92, 440–445.
- Zehnder M, Gold SI, Hasselgren G. Pathologic interactions in pulpal andperiodontal tissues. J Clin Periodontol 2002; 29: 663–671.
- Bergenholtz G, Nyman S. Endodontic complications following periodontal and prosthodontic treatment of patients with advanced periodontal disease. J Periodontol 1984; 55: 63–68.
- Jaoui L, Machtou P, Ouhayoun JP. Long-term evaluation of endodontic and periodontal treatment. Int Endod J 1995; 28: 249–254.
- Papapanou PN, Sanz M, Buduneli N, Dietrich T, Feres M, Fine DH, Flemmig TF, Garcia R, Giannobile WV, Graziani F, Greenwell H, Herrera D, Kao RT, Kebschull M, Kinane DF, Kirkwood KL, Kocher T, Kornman KS, Kumar PS, Loos BG, Machtei E, Meng H, Mombelli A, Needleman I, Offenbacher S, Seymour GJ, Teles R, Tonetti MS. Periodontitis: Consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol. 2018 Jun;89 Suppl 1:S173-S182.
- Cortellini P, Tonetti MS. Evaluation of the effect of tooth vitality on regenerative outcomes in infrabony defects. J Clin Periodontol. 2001 Jul;28(7):672-9.
- Patel S, Foschi F, Mannocci F, Patel K. External cervical resorption: a three-dimensional classification. Int Endod J. 2018 Feb;51(2):206-214.

Fig. 1: A challenging clinical presentation: Teeth #20 and #21 presented with diffuse swelling but minimal pain on percussion and bite. Both teeth did not respond to sensibility testing.
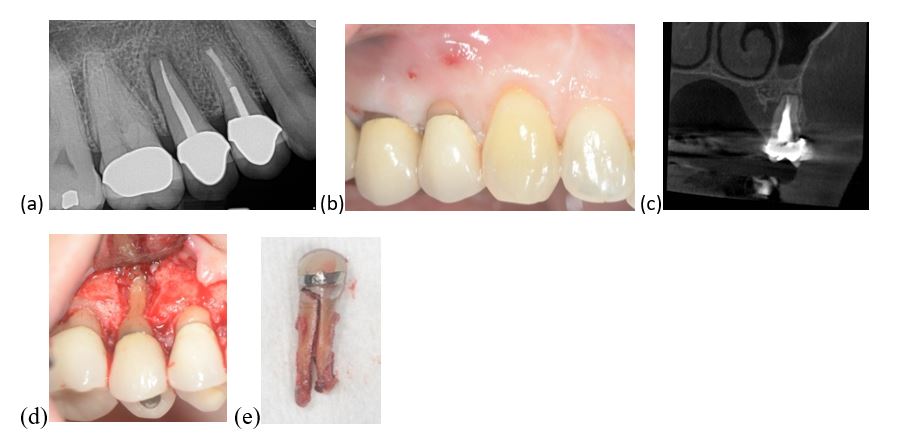
Fig. 2: Tooth #4 presented with (a) PDL widening, peri-apical radiolucency, (b) deep isolated pocket mid-buccally and a draining fistula. (c) A CBCT scan showed a J-shaped lesion. The suspicion of a vertical root fracture (VRF) is high, which was also confirmed via a diagnostic flap (d). (e)Teeth with VRF have a hopeless prognosis and need to be extracted.
Dr. Sami Chogle is Chair and Program Director, Department of Endodontics, Boston University Henry M. Goldman School of Dental Medicine. Dr. Pinelopi Pani is Clinical Associate Professor, Boston University Henry M. Goldman School of Dental Medicine.
Disclaimer
The views and opinions expressed by authors are solely those of the authors and do not necessarily reflect the official policy or position of the American Association of Endodontists (AAE). Publication of these views does not imply endorsement by the AAE.
The American Association of Endodontists (AAE) is proud to be at the forefront of national coalition efforts to advance community water fluoridation (CWF), both across the United States and on U.S. military bases abroad. As an active member of the Organized Dentistry Coalition, AAE plays a pivotal role in uniting stakeholders, promoting evidence-based policy, and accelerating progress toward sustainable oral health infrastructure. Together with our partners, we are amplifying a collective voice to ensure every community—civilian and military alike—has access to the scientifically proven benefits of fluoridated water.
The AAE has strongly opposed legislative efforts this year to ban community water fluoridation in states such as Utah and Florida. These measures threaten to undermine one of the most proven, science-based public health strategies and risk setting a dangerous precedent that could inspire similar actions elsewhere. Removing fluoride from municipal water supplies would jeopardize the oral health of all Americans—particularly children and underserved populations who rely most heavily on preventive care. AAE remains unwavering in its advocacy for equitable, data-driven public health policies that preserve and advance oral health at the community level.
Community water fluoridation is widely recognized by public health authorities and the dental profession as one of the most impactful strategies for preventing dental decay. Dr. Steven Katz, President of the AAE, underscores its importance: “Fluoride strengthens enamel and reduces the need for invasive procedures, such as root canals.” The Centers for Disease Control and Prevention (CDC) attributes a 25% decline in cavities among children and adults to fluoridated water, making it a cornerstone of modern preventive care. These benefits are especially crucial for populations with limited access to dental services—such as military families stationed overseas—who depend on accessible, preventive solutions.
For military personnel and their families, oral health is more than a matter of wellness—it is a mission-critical component of overall readiness and well-being. Nearly two million beneficiaries rely on the TRICARE Dental Program, yet many overseas installations lack consistent access to on-base dental clinics, particularly for children. Fluoridated water, when combined with fluoride toothpaste, provides essential dual protection that cannot be easily replicated. Historical guidance from the Department of Defense (DoD) has consistently affirmed the necessity of maintaining optimal fluoride levels in water systems to support health and operational effectiveness. Eliminating this resource risks increasing dental disease rates and compromising deployability, especially among junior enlisted personnel.
AAE remains steadfast in its coalition efforts and joins the Organized Dentistry Coalition in strongly urging the Department of Defense to maintain the current standard of 0.7 mg/L of fluoride in all overseas military water systems. Upholding this standard is critical not only to protecting the health of service members and their families but also to preserving mission readiness and controlling healthcare costs across systems like TRICARE.
Together, we must continue to advocate for forward-thinking, evidence-based policies that ensure oral health equity and protect the hard-won public health gains of the past century.
Compiled by Rae Burach
This is the story behind a historic and significant piece of footage—believed to be the first-ever recording of a root canal treatment.
The footage was brought to AAE’s attention by Dr. Brad Gettleman after being passed along by Dr. Ben Johnson. We spoke with both about why the footage must continue to be shared and the insights it offers into the evolution of endodontic care. More than just a glimpse into the past, this footage invites reflection on how far the field has come and what we can still learn from these early moments captured on film.
Rae Burach: How did you acquire this historic footage?
Dr. Ben Johnson: I got it from Jacob Freedland, the 22nd Past President of the AAE (1964). He got it from Edwin C. Van Valey, the 25th Past President (1967), whose father practiced with M. L. Rhein in New York City. Freedland called me up and said, “I have this old film of a guy doing a root canal—could you restore it for us?” At the time it was the late 80s, early 90s. I got hold of a guy in California who was in the movie business. When I shipped it to him, he said, “Whoa, this is on nitrate film. This is from the early 1900s and could explode when we open the canister, so they charged me $10,000 just to open it! Then he called me back and said the film is actually in pretty good shape and he could convert it to video. At one point in time, I had it on a DVD playing in my office, so people in the waiting room would see it and go, “You’re not going to do it that way, are you?” No, no, no; that’s the way it was done 100 years ago.
Burach: What was your reaction when you first watched this footage? What stood out to you most about Dr. Rhein’s technique or equipment?
Dr. Johnson: Several things! He used the same contra-angle that I used in dental school. Of course, I went to school in the 1960s, but it’s pretty similar to the contra-angles we use today. The wide brush for cleaning off the burs—that was in the Union Broach catalog and may still be, for all I know! 1917 was before files were invented; k-files didn’t come out until 1919, so in 1917 they used apical picks. I found out that M. L. Rhein also developed an instrument that was a little bit oval—it was not circular because he knew canals were not circular—and that was innovative. He took two or three appointments to do those root canals he did in the film whereas now, most endos do things in one sitting or maybe two, but I was very impressed. It was cool to see that the principles of endodontics don’t change. Techniques do, but principles don’t. In part of that film, you see a woman putting some instruments into a cylinder-looking thing on a tray and starting a stopwatch. Our methods of sterilizing with autoclaves generally take 30-45 minutes. In the early 1900s, instruments were only sterilized for like 15-20 seconds. But I don’t discount what they were doing because that was a big time for bacteriology. And of course, this is decades before antibiotics, so you did what you could to avoid infection.
Dr. Brad Gettleman: The first thing that stood out to me about the video was that the “essentials for success” listed at the beginning are virtually the same as those we recognize today. Another early reaction I had was just how similar endodontic treatment remains compared to over 100 years ago. We’re still using many of the same foundational principles—such as isolation techniques, irrigating solutions, and obturation materials. It’s remarkable to consider that while a 12-month-old cell phone is practically obsolete, the core concepts of endodontic therapy have endured for more than a century. Of course, our instruments and materials have improved significantly, but the fundamental similarities are striking. What impressed me most about Dr. Rhein’s treatment was how remarkably effective it was, especially given the limited instrumentation available to him at the time. Also, the emphasis on disinfection was also quite evident—from the use of “bichloride solution” to the application of “ionization” to eliminate all “pathogenic focus.”
Burach: Given your experience in endodontics, what lessons have you drawn from this footage, or what can today’s and future clinicians draw from it?
Dr. Johnson: When I went through graduate school it was 1971 to 1973. We didn’t become a specialty until 1964, so we were still in our first decade. I had to read all the literature ever published about endodontics going back to the 1800s, so what’s in this video isn’t necessarily new to me, but it’s informative. In the late 1980s I videotaped some procedures because it’s so much more informative than just slides, but getting things organized to videotape and go seamlessly without too many cuts—that’s very difficult. I can only imagine how difficult it was for Rhein to do on film in 1917. I was very impressed. Rhein was just one of about a half dozen men who were well known at that point in history for doing endodontics. I’ve always given copies away to colleagues who ask or direct them to wherever it is online. I think it’s important for us to know where we came from. It gives you a perspective of where you are and an insight into where you’re going.
Dr. Gettleman: As an educator, I can use the video to introduce a lecture or seminar on the history of endodontics. It can be used to discuss the challenges faced by early practitioners, including limited instruments, rudimentary asepsis, and less scientific understanding. It highlights Dr. Rhein’s pioneering efforts and how early attempts laid the groundwork for modern techniques. I can assign students to compare Dr. Rhein’s techniques with current best practices and ask them to identify elements that have remained conceptually consistent versus those that have dramatically changed. We can focus on the focal infection theory, which was widely accepted in Rhein’s era and contributed to the extraction of many restorable teeth. This helps students see continuity in clinical thinking despite technological advances.
Burach: How does this footage add to our understanding of the evolution of root canal therapy?
Dr. Gettleman: Diagnosis and Imaging: Dr. Rhein relied solely on clinical signs and rudimentary radiographs to make a diagnosis. Endodontic diagnosis has advanced significantly since that time, with the advent of digital radiography, CBCT (cone beam computed tomography), electric pulp testing, and thermal testing, allowing for more precise localization and assessment of pulpal and periapical conditions.
Instrumentation: Dr. Rhein used hand files (not finger files)—which were unstandardized, difficult to use, and prone to breakage. Hand files have been replaced by finger files and instruments have become standardized. While instrumentation has evolved with nickel-titanium rotary and reciprocating files, which are more flexible, fracture-resistant, and efficient, improving both safety and effectiveness in shaping the canal system.
Irrigation and Disinfection: Irrigants and solutions were not nearly as efficacious as they are today. Additionally, practitioners had virtually no understanding of microbial biofilms. We now use sodium hypochlorite, EDTA, chlorhexidine, and advanced techniques such as ultrasonic activation, laser activated irrigation systems, as well as other irrigation systems to disrupt biofilms and achieve thorough disinfection.
Obturation: Obturating materials included gutta-percha, but techniques were inconsistent and often did not achieve a true seal. Sealer-cement was not used in the video! While gutta-percha remains the core material, obturation techniques have improved with thermoplasticized delivery, bioceramic sealers, and hydraulic condensation, leading to much more predictable results!
Restoration and Coronal Seal: Limited focus was placed on long-term coronal restoration, often resulting in reinfection. Emphasis on restorative endodontics has led to improved outcomes through immediate, bonded, well-sealed restorations that preserve tooth structure and prevent leakage.
Sterilization and Asepsis: Asepsis was rudimentary; sterile gloves and masks were not consistently used, and rubber dam usage was variable. However, Dr. Rhein did use a rubber dam in his video. Strict infection control protocols are standard.
Burach: In your view, what was Rhein’s most forward-thinking idea, given his time?
Dr. Gettleman: His emphasis on preserving the natural tooth through root canal therapy—at a time when extraction was the norm, particularly under the influence of the focal infection theory. He was foreshadowing the principles that now form the foundation of contemporary endodontics.
In the early 20th century, many physicians and dentists believed that infected teeth contributed to systemic illness, leading to widespread extractions—even of restorable teeth. Despite practicing in this era, Dr. Rhein promoted conservative treatment aimed at retaining the natural dentition, which aligns with modern endodontic philosophy. His use of aseptic technique, rubber dam isolation, and efforts to clean, shape, and fill the canal system showed a surprisingly modern understanding of disease control and tooth preservation.
Rae Burach is the AAE’s integrated communications specialist.
Dear Colleagues,
The Honors and Awards Committee is seeking nominations for AAE awards to be presented at AAE27 in San Antonio. As you think back on your career, is there a mentor who played an important role in your success, a researcher whose work shaped the field, an educator who inspired countless students, or an endodontist who has made exceptional contributions to the specialty, the dentistry profession and their community? Consider nominating them for an AAE award!
Nominating candidates who have influenced your practice, your science or your life is a wonderful way to show your appreciation for their contributions.
Please visit www.aae.org/awards to review the award categories; the list of past award winners; and take a moment to familiarize yourself with the revised award criteria and the updated steps to submit a nomination to the AAE.
All nominations will remain confidential and must be received before August 29, 2025. Nominations remain active for two years. Nominations received last year will remain active for consideration during this cycle and new nominations received will remain active for one additional cycle. Please note that candidates not selected previously may be re-nominated.
Many thanks for your thoughtful consideration.
Warm regards,
Keith V. Krell, D.D.S., M.S., M.A.
Honors and Awards Committee Chair
To kick off Save Your Tooth Month 2025, AAE President Dr. Steven Katz completed an impactful Satellite Media Tour on May 1, conducting more than 20 interviews across radio, television, and digital platforms. Speaking with media outlets nationwide from a New York City studio, Dr. Katz shared key findings from a new AAE survey revealing that while Americans value their teeth, many still fall short on daily hygiene habits like flossing and preventive dental visits. He ultimately tied those findings back to the important role endodontists play in oral and overall health. View clips.
Additionally, The New York Sun recently featured AAE’s survey on misinformation, and included a quote from Dr. Katz:
Last month, Dr. Katz’s interview with The Pulp Dental Podcast was published, and has thus far garnered over 21,000 views! In case you missed it, catch the episode here.