The Changing Philosophy of Root Canal Obturation

By Jianing (Jenny) He, D.M.D., Ph.D.
The advent of calcium silicate-based (CS) bioceramic sealers in recent years is driving a shift in the philosophy of obturation towards a more simplified, sealer-centric approach.
As one of the three pillars of non-surgical root canal treatment, obturation plays a critical role in ensuring the long-term success of treatment. Following thorough root canal debridement and disinfection, obturation serves to prevent bacteria, bacterial products and structural components from leaking into the periapical tissue to cause disease, as well as to prevent any nutrients in the periapical tissue from reaching any remaining intracanal bacteria. As the obturation material often directly contacts the periapical tissue, it also functions as a wound dressing to promote healing, repair, and regeneration.
The basic functions of obturation are typically achieved through the combined use of a core material and a sealer. Since its first documented use over a century ago, gutta-percha remains the dominant core material in use today. Although gutta-percha has many desirable properties as an obturation material, the most important drawback is its lack of sealing ability. Therefore, gutta-percha needs to be used with a sealer that fills the space between the core and the canal walls to provide a seal. Historically, many different types of sealers have been introduced for endodontic use. These include zinc oxide eugenol (ZOE) -based, resin-based, glass ionomer-based, silicon-based, and calcium hydroxide-containing sealers. Each of these materials has its own advantages and limitations. Most of these traditional sealers have some degree of volumetric shrinkage as they set, which limits their use in large volumes due to the potential for forming voids and gaps. Therefore, in traditional obturation techniques such as cold lateral compaction, continuous wave, or carrier-based obturation, gutta-percha is expected to occupy most of the canal space with minimal amounts of root canal sealers(1). Techniques that primarily rely on sealers to fill the canal space such as paste-only or the traditional single cone technique were not considered an acceptable or mainstream obturation technique. According to a survey conducted in 2009, only about 3% of endodontists at the time described their obturation technique as “single-cone”(2).
Over the last decade, a significant development in the field of obturation materials was the introduction of CS sealers such as EndoSequence BC sealer and BioRoot RCS. These materials share similar compositions and properties with MTA, and offer additional benefits of being non-staining, having less impurities and smaller particle sizes. In vitro studies have shown that these CS sealers have excellent flowability, adequate radiopacity, high pH, good dimensional stability and sealing ability(3-5). They are also antibacterial and highly biocompatible with the ability to induce mineralization(6-9).
The unique properties of CS sealers have allowed the clinicians to challenge the traditional gutta-percha-based philosophy of root canal obturation and have reinvented the “single-cone” concept. The excellent flow characteristics and the slight volume expansion during setting allow the sealers to be used in a relatively large volume without the concerns of void formation. The antibacterial property and biocompatibility help to reduce the risk of reinfection and promote healing. In this CS sealer-based “single-cone” technique, a pre-fitted gutta-percha cone is inserted into a sealer-filled canal space to create hydraulic pressure, driving the sealer three-dimensionally throughout the canal system to achieve a seal. No lateral or vertical compaction is needed. Therefore, the technique is also sometimes referred to as “hydraulic condensation” (10). Compared to traditional techniques, this CS sealer-based obturation is simple, efficient, and cost-effective. Like all obturation techniques, the key to achieving high quality obturation using this technique is thorough debridement and disinfection prior to obturation. Having sufficient sealer in the canal is also critical in preventing void formation in this sealer-based technique. This technique can be used to effectively obturate any canal system, not only small and curved canals. Minor modifications such as passively adding accessory cones may be needed to obturate large canals and ovoid canals.
Another important advantage of this sealer-based technique is that it is consistent with the contemporary biology and anatomy-conscious philosophy of root canal treatment. In the past decade, endodontists have become increasingly aware of the importance of preserving more tooth structure and avoiding excessive force during treatment to reduce the risk of vertical root fracture. New technology such as CBCT, microscopes, more flexible instruments and active irrigation systems allow a more conservative preparation of the canals space while maintaining the same level of disinfection. The CS sealer-based “single-cone” technique allows efficient obturation of less aggressively shaped canal spaces while avoiding any wedging force associated with lateral or vertical compaction.
The quality of obturation achieved with this simplified technique appears to be on par with the other established techniques such as cold lateral and warm vertical compaction, when judged by obturation density and the presence voids(11, 12). The ultimate criteria used to determine whether a new material or technique is appropriate for clinical application is clinical success. Clinical studies evaluating the outcomes of obturation are typically challenging to do due to the inherent difficulties in controlling other confounding variables such as the patient’s systemic conditions, pre-op diagnosis, instrumentation and irrigation protocols, and the quality of coronal restoration. As a result, few randomized controlled trials are available. At this point, only one prospective cohort study and one case series have been published on the outcomes of CS sealer-based obturation. Both studies demonstrated satisfactory clinical success comparable to the warm vertical technique(13, 14). Clinical trials examining the effects of obturation on postoperative pain also showed no significant difference between cases obturated with CS sealers and those obturated with resin-based sealers (15-17).
A recent survey shows close to 60% of practitioners world-wide are currently using some form of CS sealer-based obturation technique(18). As this technique is being embraced by more clinicians, certain questions remain. For example, large discrepancies in the literature regarding the setting time and solubility of CS sealers have raised concerns regarding the stability and long-term success of the cases obturated with these materials. In addition, clinicians continue to search for a solvent to facilitate the removal of these materials during retreatment.
In conclusion, root canal obturation is seeing a shift from traditional gutta-percha-based obturation to a more sealer-based philosophy. CS sealers like EndoSquence BC sealer and BioRoot RCS allow clinicians to obturate root canal systems using a simplified technique without compromising the quality of obturation or treatment outcome. Future clinical studies with more rigorous design, larger sample sizes, and longer follow-ups are needed to confirm the long-term success of these materials.
Figure 1: Cases obturated with the CS sealer-based technique demonstrate quality comparable to other techniques.
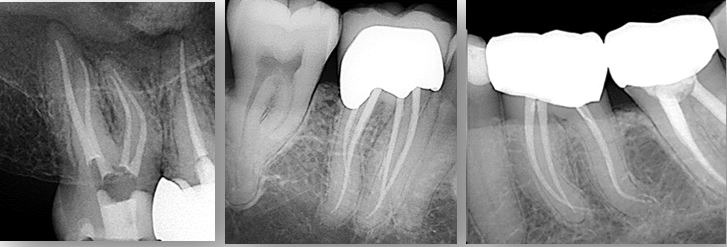
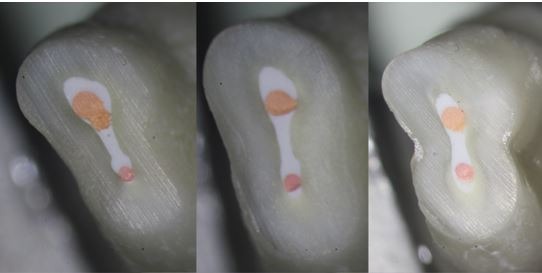
Figure 2: Cross sections of a maxillary premolar obturated with the CS sealer-based technique showing well-obturated canal space with gutta-percha cones embedded within a dense layer of sealer. Image courtesy of Dr. Martin Trope.
References:
- AAE Appropriateness of Care and Quality Assurance Guidelines. 1994.
- Lee M, Winkler J, Hartwell G, Stewart J, Caine R. Current trends in endodontic practice: emergency treatments and technological armamentarium. J Endod 2009;35(1):35-39.
- Zhou HM, Shen Y, Zheng W, Li L, Zheng YF, Haapasalo M. Physical properties of 5 root canal sealers. J Endod 2013;39(10):1281-1286.
- Candeiro GT, Correia FC, Duarte MA, Ribeiro-Siqueira DC, Gavini G. Evaluation of radiopacity, pH, release of calcium ions, and flow of a bioceramic root canal sealer. J Endod 2012;38(6):842-845.
- Ballullaya SV, Vinay V, Thumu J, Devalla S, Bollu IP, Balla S. Stereomicroscopic Dye Leakage Measurement of Six Different Root Canal Sealers. J Clin Diagn Res 2017;11(6):ZC65-ZC68.
- Zhang W, Li Z, Peng B. Effects of iRoot SP on mineralization-related genes expression in MG63 cells. J Endod 2010;36(12):1978-1982.
- Wang Z, Shen Y, Haapasalo M. Dentin extends the antibacterial effect of endodontic sealers against Enterococcus faecalis biofilms. J Endod 2014;40(4):505-508.
- Giacomino CM, Wealleans JA, Kuhn N, Diogenes A. Comparative Biocompatibility and Osteogenic Potential of Two Bioceramic Sealers. J Endod 2019;45(1):51-56.
- Ricucci D, Grande NM, Plotino G, Tay FR. Histologic Response of Human Pulp and Periapical Tissues to Tricalcium Silicate-based Materials: A Series of Successfully Treated Cases. J Endod 2020;46(2):307-317.
- Koch KA, Brave DG, Nasseh AA. Bioceramic technology: closing the endo-restorative circle, Part I. Dent Today 2010;29(2):100-105.
- Holmes S, Gibson R, Butler J, Pacheco R, Askar M, Paurazas S. Volumetric Evaluation of 5 Root Canal Obturation Methods in TrueTooth 3-dimensional-Printed Tooth Replicas Using Nano-computed Tomography. J Endod 2021;47(3):485-491 e484.
- Roizenblit RN, Soares FO, Lopes RT, Dos Santos BC, Gusman H. Root canal filling quality of mandibular molars with EndoSequence BC and AH Plus sealers: A micro-CT study. Aust Endod J 2020;46(1):82-87.
- Chybowski EA, Glickman GN, Patel Y, Fleury A, Solomon E, He J. Clinical Outcome of Non-Surgical Root Canal Treatment Using a Single-cone Technique with Endosequence Bioceramic Sealer: A Retrospective Analysis. J Endod 2018;44(6):941-945.
- Zavattini A, Knight A, Foschi F, Mannocci F. Outcome of Root Canal Treatments Using a New Calcium Silicate Root Canal Sealer: A Non-Randomized Clinical Trial. J Clin Med 2020;9(3).
- Aslan T, Donmez Ozkan H. The effect of two calcium silicate-based and one epoxy resin-based root canal sealer on postoperative pain: a randomized controlled trial. Int Endod J 2021;54(2):190-197.
- Tan HSG, Lim KC, Lui JN, Lai WMC, Yu VSH. Postobturation Pain Associated with Tricalcium Silicate and Resin-based Sealer Techniques: A Randomized Clinical Trial. J Endod 2021;47(2):169-177.
- Yu YH, Kushnir L, Kohli M, Karabucak B. Comparing the incidence of postoperative pain after root canal filling with warm vertical obturation with resin-based sealer and sealer-based obturation with calcium silicate-based sealer: a prospective clinical trial. Clin Oral Investig 2021;25(8):5033-5042.
- Guivarc’h M, Jeanneau C, Giraud T, Pommel L, About I, Azim AA, et al. An international survey on the use of calcium silicate-based sealers in non-surgical endodontic treatment. Clin Oral Investig 2020;24(1):417-424.
Dr. Jenny He is clinical associate professor, Department of Endodontics, Texas A&M University College of Dentistry, and a member of the Journal of Endodontics’ Editorial Board Committee.




