To Scan or Not to Scan, That is the Question
By Dr. Mohamed Fayad
 To scan, or not to scan, that is the question? Is there a straightforward case? These are some of the common questions that endodontists face in their daily practices. In endodontics, clinical examination and diagnostic imaging are both essential components of the preoperative diagnosis. Cone Beam Computed Tomography is a diagnostic imaging modality that provides high-quality, accurate 3-D representations of the osseous elements of the maxillofacial skeleton. CBCT has great potential to become a valuable tool in modern endodontic practice. The addition of subjective and objective clinical findings to CBCT should allow for an even more accurate clinical diagnosis and appropriate treatment plan. Accurate diagnosis leads to confident treatment planning, which is an integral part of the endodontic decision-making process. Conventional 2-D radiographs continue to be the most popular method of imaging today. However, the diagnostic potential of periapical radiographs is limited.
To scan, or not to scan, that is the question? Is there a straightforward case? These are some of the common questions that endodontists face in their daily practices. In endodontics, clinical examination and diagnostic imaging are both essential components of the preoperative diagnosis. Cone Beam Computed Tomography is a diagnostic imaging modality that provides high-quality, accurate 3-D representations of the osseous elements of the maxillofacial skeleton. CBCT has great potential to become a valuable tool in modern endodontic practice. The addition of subjective and objective clinical findings to CBCT should allow for an even more accurate clinical diagnosis and appropriate treatment plan. Accurate diagnosis leads to confident treatment planning, which is an integral part of the endodontic decision-making process. Conventional 2-D radiographs continue to be the most popular method of imaging today. However, the diagnostic potential of periapical radiographs is limited.
The different applications of CBCT in diagnosis, treatment planning and long-term outcome evaluation are well documented in the endodontic literature (1-8). In 2015, a revised joint AAE/AAOMR position statement on the use of limited field of view CBCT in endodontics was published (9).
The impact of CBCT in nonsurgical and surgical treatment planning was evaluated in several recent studies (10-12). A recently published prospective observational study evaluated the outcome of CBCT examinations performed in a clinical setting and the impact on diagnosis before CBCT examination (Stage 1) and after CBCT examination (Stage 2) (10). The results of the study demonstrated a change in diagnosis in 22 patients (42 percent) between Stage 1 and Stage 2. Treatment planning decisions using CBCT versus intraoral radiographs were compared to the gold standard diagnosis (11). An accurate diagnosis was reached in 36.6 percent to 40 percent of the cases when using periapical radiographs compared to an accurate diagnosis in 76.6 percent to 83.3 percent of the cases when using CBCT. The previous study also demonstrated that the treatment plan may be directly influenced by information gained from a CBCT scan as the examiners altered their treatment plan after viewing the CBCT scan in 62.2 percent of the cases overall (ranging from 56.6 percent to 66.7 percent). In a recent study, the influence of CBCT imaging on clinical decision-making choices among different specialists (prosthodontists, endodontists, oral surgeons, and periodontists) in endodontic treatment planning was evaluated (12). CBCT imaging had a substantial impact on endodontic decision making among specialists, particularly in high-difficulty cases. After viewing the CBCT scan, the extraction option increased significantly (P < .05).
The previous studies indicated that CBCT had a significant influence on the examiner’s treatment plan. The problem of incorrect, delayed or inadequate endodontic diagnosis and treatment planning places the patient at risk and could result in unnecessary or inappropriate treatment.
Important information that can be visualized in CBCT imaging, such as canal transportation and the extent of the root canal filling, may be difficult to interpret on a 2-D radiograph. The additional information obtained from CBCT can be a key determining factor in the decision making process.
Although imaging is a very important diagnostic tool in endodontics, it should always be used as an adjunct to the clinical exam. The addition of subjective and objective clinical findings to CBCT should allow for an even more accurate clinical diagnosis and appropriate treatment plan. Cases 1 through 3 are examples of utilizing CBCT imaging in diagnosis and its impact on treatment planning cases with pre- and post-treatment symptoms and pathology.
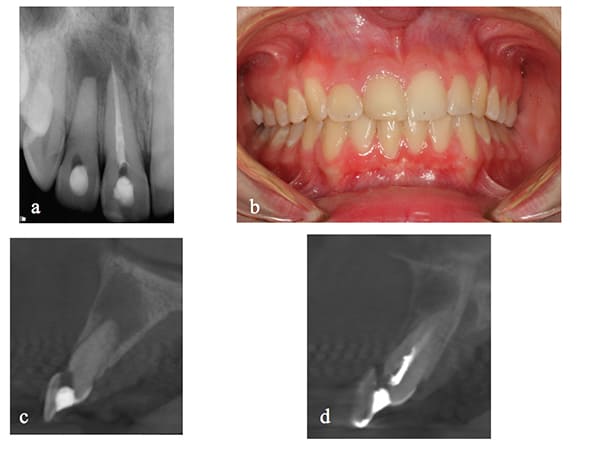
Case No. 1, Figure 1: 1: (a) Periapical radiograph of teeth 7 and 8. Treatment was initiated on both teeth before referral to an endodontist. (b) Clinical picture showing normal soft tissue color and architecture. (c) and (d) are sagittal CBCT images showing facial perforations on teeth 7 and 8, respectively.
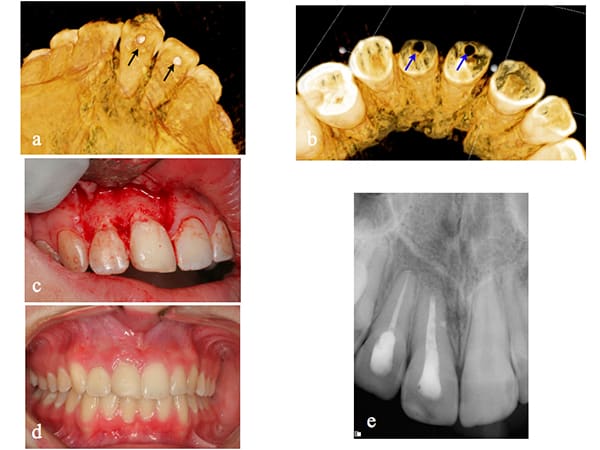
Figure 1:2: Continuation of Case 1: (a) and (b) are 3D reconstructions showing the facial perforations on teeth 7 and 8. (c) Reflection of a full-thickness mucoperiosteal flap confirmed the presence of perforations on both teeth. The perforations were repaired with Geristore (DenMat, Lompoc, Calif.). Both teeth were then treated via an orthograde approach with subsequent surgical root-end resection and filling of tooth 8. (d and e) Two-year recall radiograph demonstrating soft and hard tissue healing.
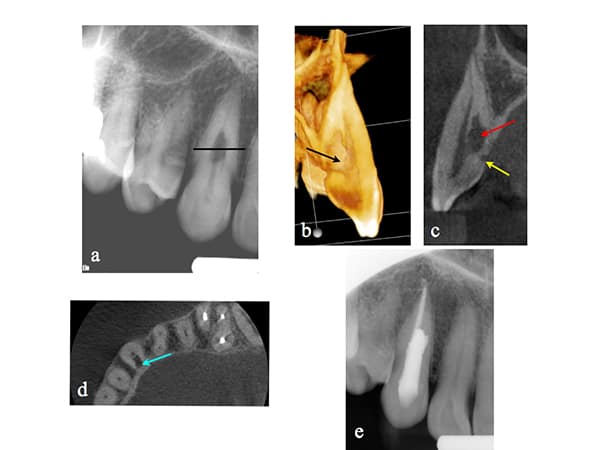
Case No. 2: (a) Periapical radiograph of tooth 6. The patient was referred for evaluation and treatment of an internal resorptive defect. The line corresponds to the axial section view in (d). (b) 3-D reconstruction of the resorptive defect (black arrow). (c) Sagittal view of tooth 6 demonstrating the internal resorptive defect (red arrow), and confirming that the defect is an external ICR defect with initial entry at the cemento-enamel junction (yellow arrow). (d) Axial view demonstrating the ICR nature of the defect. Note in (c and d) that the pulp was not involved. (e) Post-operative radiograph of tooth 6 after root canal therapy and repair of the resorptive defect.
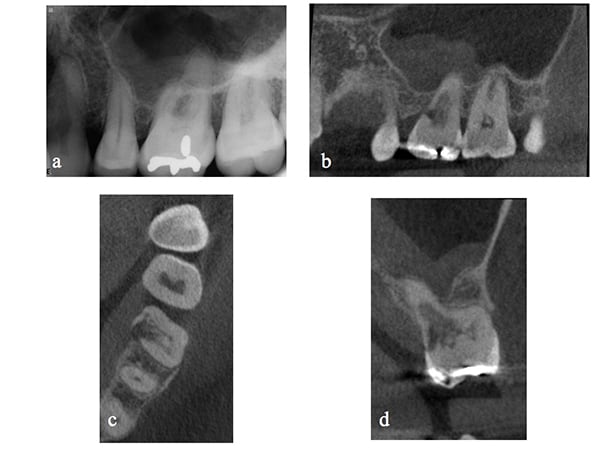
Case No. 3: (a) Periapical radiograph of tooth 14. Symptoms included spontaneous pain and abnormal sensitivity to cold. After clinical examination and testing, the diagnosis was symptomatic irreversible pulpitis with symptomatic apical periodontitis. (b) CBCT sagittal view of tooth 14 showing an invasive cervical resorptive defect (ICR – Heithersay Class IV) that cannot be detected on the periapical radiograph. (c) Axial view demonstrating the palatal and mesial location of the defect. (d) Coronal view demonstrating the internal aspect of the ICR defect, rendering tooth 14 non- restorable. A change in treatment plan was made and the patient was referred for extraction.
Dr. Mohamed I. Fayad is a clinical associate professor and director of endodontic research at the University of Illinois at Chicago College of Dentistry and is in private practice in Chicago. He can be reached at mfayad1@uic.edu.
Works Cited
- Setzer FC, Hinckley N, Kohli MR, Karabucak B. A survey of cone-beam computed tomographic use among endodontic practitioners in the United States. J Endod 2017;43:699-704.
- Lofthag-Hansen S, Huumonen S, Grondahl K, Grondahl HG, Limited cone-bean CT and intraoral radiography for the diagnosis of periapical pathology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103:114-9.
- Cotton TP, Geisler TM, Holden DT, et al. Endodontic applications of cone-beam volumetric tomography. J Endod 2007;33:1121-32.
- Patel S, Dawood A, Whaites E, Pitt Ford T. New dimensions in endodontic imaging: part 1. Conventional and alternative radiographic systems. Int Endod J 2009;42:447-62.
- Patel, S.: New dimensions in endodontic imaging: part 2. Cone beam computed tomography. Int Endod J 2009;42:463-75.
- Scarfe WC, Farman AG, Sukovic P. Clinical applications of cone-beam computed tomography in dental practice. J Can Dent Assoc 2006;72:75-80.
- Nair MK, Nair UP. Digital and advanced imaging in endodontics: a review. J Endod 2007;33:1-6.
- Schloss T, Sonntag D, Kohli MR, Setzer FC. A comparison of 2- and 3-dimensional healing assessment after endodontic surgery using cone-beam computed tomographic volumes or periapical radiographs. J Endod 2017;43:1072-9.
- Joint Position Statement of the American Association of Endodontists and the American Academy of Oral and Maxillofacial Radiology on the Use of Cone Beam Computed Tomography in Endodontics 2015 Update.
- Mota de Almeida FJ, Knutsson K, Flaygare L. The impact of cone beam computed tomography on the choice of endodontic diagnosis. Int Endod J, 48,564–572, 2015.
- Ee J, Fayad MI, Johnson BR. Comparison of endodontic diagnosis and treatment planning decisions using cone-beam volumetric tomography versus periapical radiography. J Endod. 014;40:910-6.
- Rodriquez G, Abella F, Duran-Sindren F, Patel S, Roig M. Influence of Cone-beam Computed Tomography in Clinical Decision Making among Specialists. J Endod 2017;43:194–199.




