Traumatic Pulp Exposures: A Quick Review

By Dr. Joseph Stern
Introduction:
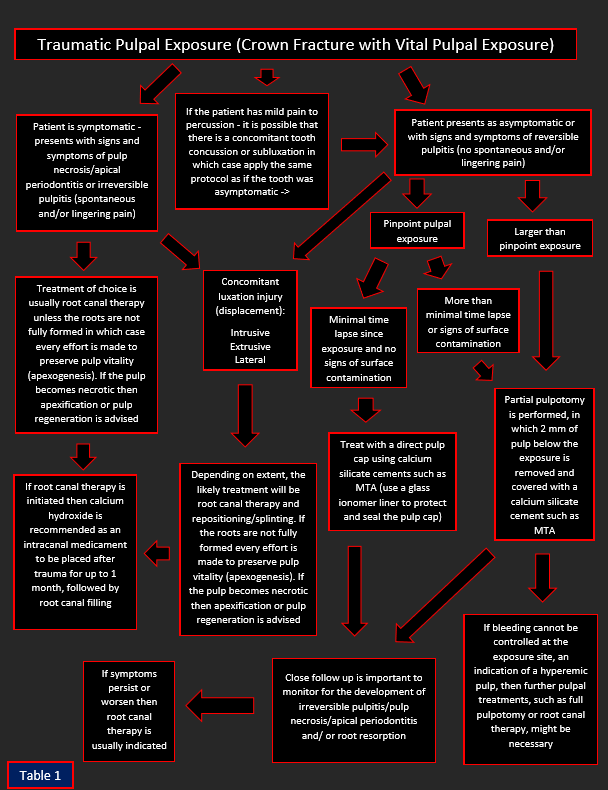
There are many important questions to consider prior to treating a traumatic pulpal exposure (see table 1). How long has the exposure been present? The longer the exposure has been present the higher the likelihood for bacterial contamination of the pulp. However, as long as the pulp is still vital and the patient’s symptoms don’t necessitate root canal therapy, vital pulpal treatments can be employed. Is the patient symptomatic? What are the pulpal and periapical diagnoses? The pulpal and periapical diagnosis will dictate treatment. For example, if the pulpal diagnosis is necrosis or irreversible pulpitis (spontaneous or lingering pain) then pulpectomy (root canal therapy) is usually indicated rather than a vital pulpal treatment such as a pulp cap or partial pulpotomy.
A tooth with periapical pathology is usually not a good candidate for vital pulpal treatments. A proper diagnosis must be reached before deciding to perform vital pulpal treatments. Vital pulpal treatments will usually not work if the pulp is severely inflamed or infected. Is there a concomitant luxation injury or root fracture? A concomitant laxation injury or root fracture might further complicate pulpal circulation and thereby necessitate a full root canal rather than vital pulpal treatment. Are the roots fully developed? As a general rule we make every effort to preserve the pulp vitality of an immature tooth to allow for continued root growth (apexogenesis). It is important to remember that although vital pulpal treatments are usually the treatment of choice for immature permanent teeth, they can be performed for both mature and immature permanent teeth. How large is the fracture/exposure? There are different levels of vital pulpal therapy, ranging from a direct pulp cap to a full pulpotomy. The size of the exposure will play a role in dictating which vital pulpal treatment is best. There are times where a fracture might compromise significant tooth structure necessitating a post (for retention of a core) in which case endodontic treatment is indicated even when the pulp is vital and the exposure is relatively small.
Table 1
Definition:
Vital pulp therapy (VPT) techniques are means of preserving the vitality and function of the dental pulp after injury resulting from trauma, caries, or restorative procedures. VPT procedures have traditionally included indirect or direct pulp capping, and partial or complete pulpotomy. VPT’s includes removal of part of the pulp allowing the rest of the pulp to remain vital and functional. We assume that by removing a small portion of the superficial inflamed pulp the remaining pulp remains healthy. When the pulp is exposed, bacterial invasion can be resisted by both the patient’s immune system present within the pulp, and the bathing of the area by the patient’s saliva which prevent impaction of contaminated debris/bacteria. While the pulp is a low compliant environment, making it more vulnerable to injury, it also has the ability to heal itself. Vital pulpal therapy is built upon this very important principle. Overall VPT has been shown to have a very high success rate.
Objective:
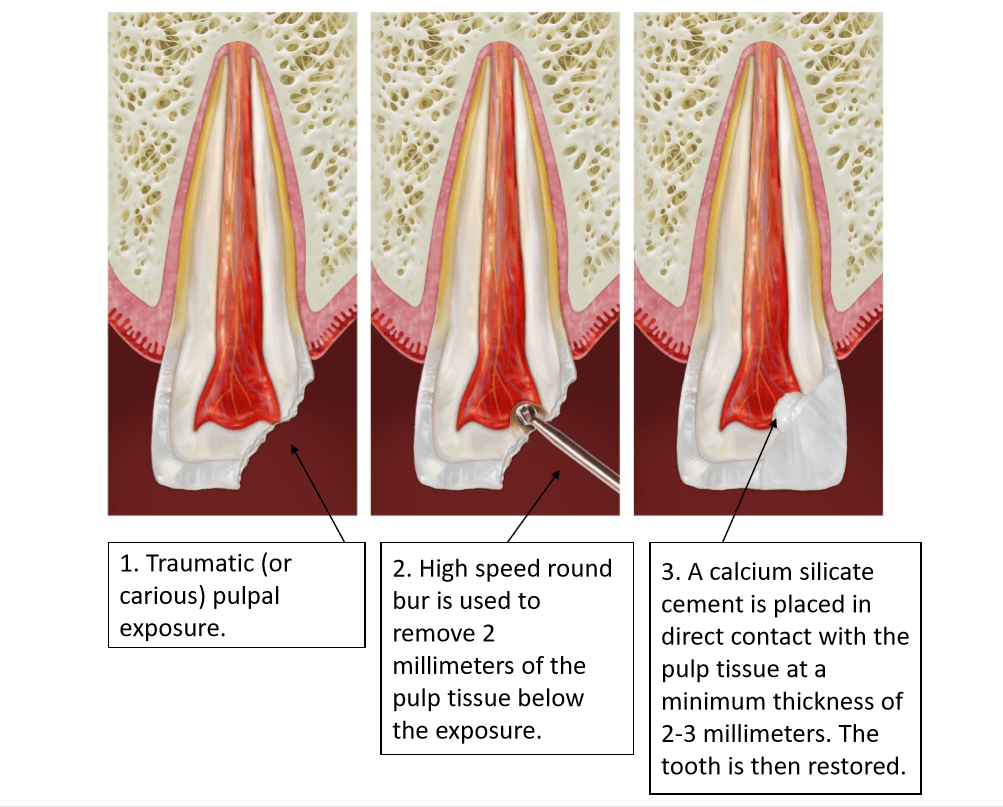
There are two essential objectives for treatment of the vital pulp that make the level of pulpal amputation important: a wound dressing should be placed on non-inflamed tissue, and the loss of tooth structure should be kept to a minimum. In crown-fractured teeth, showing vital pulp tissue after an exposure, not more than 2 mm of the pulp beneath the exposure needs to be removed (see figure 1).
Figure 1
Partial Pulpotomy vs. Direct Pulp Cap
The advantage of partial pulpotomy (removing 2 mm of coronal pulp) as compared with pulp capping lies in better control of the surgical wound and retention of the sealing material. Capping of the pulp is recommended only when the exposure is small (less than 1 mm in size) and when it can be treated shortly after the accident. These indications apply to only a limited number of teeth and, in the majority of cases, partial pulpotomy is therefore performed. It is also noteworthy that most studies find a much higher success rate with partial pulpotomy compared to pulp capping after a traumatic pulpal exposure, the reason being the better control of superficial inflammation below the exposure. It has been clearly shown that as time elapses (from 1 hour to 7 days) after injury the success of pulp capping significantly decreases (from 93% to 56%). Vital pulpal treatments can be used as a permanent treatment modality for mature and immature permanent teeth with complicated crown fractures, and re-entering of the pulp at a later time is not necessary as long as the pulp remains vital.
Hemostasis:
Sodium hypochlorite is an antimicrobial solution that provides hemostasis, disinfection of the dentin pulp interface, biofilm removal, chemical removal of the blood clot and fibrin, and clearance of dentinal chips along with damaged cells at the mechanical exposure site. Therefore, sodium hypochlorite can be used to disinfect the exposure site during a pulpotomy prior to restoring the pulpal wound (saline or chlorhexidine can be used as well). A cotton-soaked pellet is placed on the pulpal wound with pressure for this purpose.
Examination of pulp tissues after exposure is a critical step in pulp assessment. Controlled bleeding (complete hemostasis) is needed for successful partial pulpotomy. If hemostasis cannot be achieved this is an indicator that the pulp is inflamed and should not be capped. On occasion more pulp tissue needs to be removed to achieve hemostasis, and what was initially planned as a partial pulpotomy might turn into a full pulpotomy. A pulpal diagnosis of necrosis (non-vital pulp) or the inability to achieve hemostasis would obviously preclude vital pulpal treatments such as pulp cap or pulpotomy (partial or full).
Calcium Silicate Cements:
There have been few materials as groundbreaking in endodontics as MTA (mineral trioxide aggregate). This material, developed by Torabinejad in 1993, was the first of the CSC’s (calcium silicate cements), and was initially introduced for the purpose of sealing root perforations. Overtime they were found to be so biocompatible and successful in their applications that they have become mainstreamed for the use of apexogenesis, apexification, apicoectomies, and to seal root perforations. CSC’s are a class of materials that include tricalcium silicates, dicalcium silicates, hydraulic calcium silicate cements, and ‘bioceramics’ (MTA, TheraCal, Brasseler RRM, BC sealer and Biodentine are some examples). CSC’s have become more commonplace for use in vital pulp therapy (VPT) procedures. These materials are placed directly on the pulpal wound (see figure 1). While calcium hydroxide has classically been used for vital pulpal treatments most current studies clearly demonstrate that CSC’s are superior in terms of healing and success rates and are the preferred material to place on a pulpal exposure (once hemostasis is achieved). MTA was the first of these materials introduced for this purpose but newer materials have recently flooded the market. One of the advantages of the newer materials is that they don’t cause significant tooth discoloration, which can be beneficial, especially when used in the esthetic zone.
Conclusion:
When treatment planned correctly, vital pulpal treatments, such as partial pulpotomy, can be a valuable option with a high success rate. They can be utilized successfully not only for traumatic pulpal exposures but for carious pulpal exposures as well. The key to this high success rate is proper diagnosis and a well-sealed restoration above the capping material. Bacterial leakage ultimately can cause any vital pulpal treatment to fail.
A successful follow up to vital pulpal therapy would be dentin bridge formation, continued root development, positive response to pulp vitality testing, no symptoms, and no radiographic development of apical periodontitis or root resorption.
References:
AAE Position Statement on Vital Pulp Therapy, May 2021
Cvek M, Cleaton-Jones PE, Austin JC, Andreasen JO. Pulp reactions to exposure after experimental crown fractures or grinding in adult monkeys. J Endod. 1982 Sep;8(9):391
Cvek M. Partial pulpotomy in crown fractured incisors: results 3 to 15 years after treatment. Acta Stomatol Croat 1993;27:167–73.
Cvek, M. A clinical report on partial pulpotomy and capping with calcium hydroxide in permanent incisors with complicated crown fracture. J Endod 4:232-237, 1978.
Lin LM et al. Vital pulp therapy of mature permanent teeth with irreversible pulpitis from the perspective of pulp biology. Aust Endod J. 2020;46:154-165.
Bimstein E, Rotstein I. Cvek pulpotomy-revisited. Dent Traumatol 2016;32:438–42.
Fong CD, Davis MJ. Partial pulpotomy for immature permanent teeth, its present and future. Pediatr Dent 2002;24:29–32.
Heide S, Kerekes K. Delayed direct pulp capping in permanent incisors of monkeys. Int Endod J 1987; 20:65–74.
Fuks AB, Bielak S, Chosak A: Clinical and radiographic assessment of direct pulp capping and pulpotomy in young permanent teeth, Pediatr Dent 4:240, 1982.
Barthel CR, Rosenkranz B, Leuenberg A, Roulet JF. Pulp capping of carious exposures: treatment outcome after 5 and 10 years: a retrospective study. J Endod. 2000 Sep;26(9):525-8.
Dammaschke T, Leidinger J, Schäfer E. Long-term evaluation of direct pulp capping–treatment outcomes over an average period of 6.1 years. Clin Oral Investig. 2010 Oct;14(5):559-67
Cox CF, Bergenholtz G, Fitzgerald M, Heys DR, Heys RJ, Avery JK, Baker JA. Capping of the dental pulp mechanically exposed to the oral microflora — a 5 week observation of wound healing in the monkey. J Oral Pathol. 1982 Aug;11(4):327-39
Cvek M, Lundberg M. Histological appearance of pulps after exposure by a crown fracture, partial pulpotomy, and clinical diagnosis of healing. J Endod 1983;9:8–11.
Hafez AA, Cox CF, Tarim B et al. An in vivo evaluation of hemorrhage control using sodium hypochlorite and direct capping with a one- or two-component adhesive system in exposed nonhuman primate pulps. Quintessence Int. 2002;33:261-272
Cho S-Y et al. Prognostic factors for clinical outcomes according to time after direct pulp capping. J Endod. 2013;39(3):327-331
Parirokh M et al. Mineral Trioxide Aggregate: A Comprehensive Literature Review—Part III: Clinical Applications, Drawbacks, and Mechanism of Action, Journal of Endodontics, Volume 36, Issue 3, 400 – 413
Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review–Part I: chemical, physical, and antibacterial properties. J Endod. 2010 Jan;36(1):16-27.
Fuks AB, Cosack A, Klein H, Eidelman E. Partial pulpotomy as a treatment alternative for exposed pulps in crown fractured permanent incisors. Endod DentTraumatol 1987, June;3:100-2.
de Blanco LP.Treatment of crown fractures with pulp exposure. Oral Surg OralMed Oral Pathol Oral Radiol Endod 1996;82:564-8.
Nair PN, Duncan HF, Pitt Ford TR, Luder HU. Histological, ultrastructural and quantitative investigations on the response of healthy human pulps to experimental capping with mineral trioxide aggregate: a randomized controlled trial. Int Endod J. 2008 Feb;41(2):128-50.
Elmsmari F, Ruiz X-F, Miro Q, et al. Outcome of partial pulpotomy in cariously exposed posterior permanent teeth: a systematic review and meta-analysis. J Endod 2019;45:1296–1306.e3.
Mejare I, Cvek M: Partial pulpotomy in young permanent teeth with deep carious lesions, Endod Dent Traumatol 9:238, 1993.
Fuks A, Gavra S, Chosak A. Long-term follow-up of traumatized incisors treated by partial pulpotomy. Pediatric Dentistry 1993;15:334–6.
Sabeti M, Huang Y, Chung YJ, Azarpazhooh A. Prognosis of Vital Pulp Therapy on Permanent Dentition: A Systematic Review and Meta-analysis of Randomized Controlled Trials. J Endod. 2021 Sep 1:S0099-2399(21)00602-6.
Dr. Stern is a Diplomate of the American Board of Endodontics. He is the director of endodontics at the Touro College of Dental Medicine and frequently lectures on clinical endodontics. He has lectured at local county dental societies, the New Jersey Dental Association Annual Session, and the Greater New York Dental Meeting. He maintains a private practice, Clifton Endodontics, in Clifton, NJ. He can be reached at jstern5819@gmail.com or via the Instagram handle @the_barbed_broach1.
Note: This article has been adapted from an earlier version Dr. Stern authored for Dentistry Today.




