Another Tool in the Toolbox: Autotransplantation of Teeth
 By Mitsuhiro Tsukiboshi, D.D.S., Ph.D.
By Mitsuhiro Tsukiboshi, D.D.S., Ph.D.
If you ask dental professionals if they have heard of autotransplantation of teeth, many would say no. It is not taught in most dental school curriculum. However, it can be a great treatment alternative for a patient and provide successful patient outcomes.
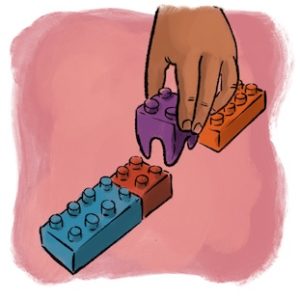
The aim of autotransplantation of teeth (ATT) is to replace a lost tooth with a functional tooth within the same patient by transplanting a tooth from one site to another. One of the first records of an ATT procedure was by a French physician, Pierre Fauchard, in his book Le Chirurgien Dentiste published in 1728, in which he surgically moved a tooth from one site to another in the same individual (1). In the early 1950s, ATT gained some more popularity and was used to replace decayed first molars with impacted, immature third molars (2–7). The success rates were fairly low (around 50%) and thus fell out of favor (8). However, with improvement in biological understanding, technology and technique, the clinical and experimental studies on ATT over the last 40 years have shown that it can be a more predictable treatment option providing successful long-term outcomes (9,10,11).
There are several important factors for successful ATT. The donor tooth must have a viable, healthy periodontal ligament so that it can successfully heal in the recipient site. Studies and clinical cases show that one can transplant a tooth into an edentulous site (i.e. site where there has not been a tooth present there before or was extracted long ago), but transplanting the donor into a socket where there is still PDL in the extraction socket may have more favorable healing of the PDL (12). Minimizing the damage and dry time to the donor tooth is also important. If the PDL is compromised or damaged during the surgical procedures or healing process, several types of root resorption may develop. The shape and size of the donor tooth should be able to fit in the dimensions of the transplant site. Having a conical root form will likely be easier and less traumatic to luxate out of the socket compared to a diverging, multi-rooted, long, curved root. If the donor tooth is immature (i.e. open apices), having the tooth in stage 4-5 root development appears to be ideal because the tooth can revascularize and the root may continue to develop (10,11). If the donor tooth is mature, there is a high likelihood of pulp necrosis due to the constricted apices, so endodontic treatment will likely be required. One can think of it as an avulsed tooth in a trauma case, which most endodontists have a familiar mental model with.
As the dental landscape continues to change, it is important that endodontists become more involved in helping the patient in their oral health outcomes. With the AAE promoting the Worth Saving campaign, more patients and dental colleagues will likely be looking to endodontists as the person who can make it happen. Thus, it is beneficial to have more than just one or two tools in the toolbox. We can provide “other” great services for the patients such as ATT, root amputations, rapid extrusion, and intentional replantation to help patients retain their own natural dentition. The overall risk is low because many times ATT is performed on a donor tooth that is “extra” and not in function (i.e. an impacted 3rd molar) and the benefit can be great. It may not be something you do every day, but there are perhaps many teeth that could be saved with favorable long-term outcomes (13). Autotransplantation of teeth is a great tool to have in the toolbox.
Reference
- Pape HD, Heiss R. History of tooth transplantation. Fortschr Kiefer Gesichtschir. 1976;20:121-125.
- Apfel H:Autoplasty of enuculeated prefunctional third molars, J Oral Surg (Chic) 1950;8(4):289-296
- Apfel H:Transplantation of the unerupted third molar tooth, Oral Surg Oral Med Oral Pathol 1956;9(1):96-98.
- Miller H M:Transplantation. J Am Dent Assoc 1950;40(2):237, illust.
- Miller H M:Tooth transplantation. J Oral Surg (Chic) 1951;9(1):68-69.
- Collings G J:Dual Transplantation of third molar tooth. Oral Surg Oral Med Oral Pathol 1951;4(10):1214-1219.
- Hale M L:Autogenous transplant. Oral Surg Oral Med Oral Pathol 1956;9(1): 76-83
- Natiella J, Armitage J, Greene G: The replantation and transplantation of teeth. Oral Surg 1970;29:397.
- Andreasen J O:Atlas of replantation and transplantation of teeth. Philadelphia: W B Saunders, 1992;111-75.
- Andreasen JO, Paulsen HU, Yu Z, Bayer T, Schwartz O:A long term study of 370 autotransplanted premolars. Part Ⅱ. Tooth survival and pulp healing subsequent to transplantation. Eur J Orthod 1990;12(1):14-24.
- Andreasen JO, Paulsen HU, Yu Z, Bayer T:A long term study of 370 autotransplanted premolars. Part Ⅳ. Root development subsequent to transplantation. Eur J Orthod 1990;12(1):38-50.
- Tsukibosi M. Autotransplantation of teeth. Chicago: Quintessence;2001;22-30, 151-67
- Tsukiboshi M, Yamauchi N, Tsukiboshi Y: Long-term outcomes of autotransplantation of teeth: A case series. Dent Traumatol. 2019;00:1-10.
Dr. Mitsuhiro Tsukiboshi, D.D.S., Ph.D., is in private practice in Aichi, Japan, and is past president of IADT. He is considered the world’s leading authority on autotransplantation of teeth. He can be reached at moonstar@guitar.ocn.ne.jp.




