Are We Maximizing Success with Minimally Invasive Endodontics?
By Drs. Anil Kishen and Meetu Kohli
The evolution of endodontics has seen a paradigm shift from traditional, more aggressive approaches to those emphasizing the preservation of tooth structure. Minimally invasive endodontics seeks to conserve the dentin and natural biomechanical structure of the tooth while maintaining or improving clinical outcomes. This article distills the essence of the 2025 AAE presentation by Drs. Kishen and Kohli, which explored the biological, biomechanical, and clinical consequences of minimally invasive approaches in endodontic treatment.
Defining Minimally Invasive Technique
The term minimally invasive originates from the medical field, particularly in reference to laparoscopic, keyhole, and robotic surgeries, which serve as alternatives to traditional open surgical approaches. The primary advantages of minimally invasive procedures such as those for gallbladder removal, hysterectomy, hernia repair, cardiac interventions, or joint surgery are centered on the reduced size of the surgical incision and, consequently, the wound itself. Numerous meta-analyses have demonstrated that minimally invasive surgery is associated with less postoperative pain, improved quality of life, a lower incidence of complications and infections, quicker recovery times, and shorter hospital stays [1]. However, the limited surgical access inherent to these techniques may hinder tactile feedback and reduce visibility of the operative field. Therefore, systematic reviews have also evaluated whether the clinical outcomes of minimally invasive approaches are comparable to those of open surgery, as any compromise in outcome would represent a significant limitation [2].
In the context of endodontics, the biological objective of treatment is to prevent and treat apical periodontitis while preserving the long-term function, aesthetics, and health of the tooth and surrounding structures. As apical periodontitis is a microbial/biofilm-associated disease, successful treatment relies on effective disinfection of the root canal system, proper obturation, and restoration. However, achieving these goals necessitates access, instrumentation, and preparation of the canal system, all of which involve removal of dentin. The cumulative loss of dentin due to both caries and procedural intervention can ultimately weaken the structural integrity of the tooth, increasing the risk of fracture and potentially compromising its long-term functionality.
Understanding Dentin: A Unique Composite
Dentin, the main structural tissue of teeth, is a natural composite made of inorganic content, organic matrix, and water. Essentially, water exists in both bound and free forms. Bound water integrates tightly with mineral crystals and the collagen network, only being removed at high temperatures [3]. Free water, however, fills dentinal tubules and voids in the matrix and significantly contributes to dentin toughness [4]. Free water plays a critical role in maintaining the viscoelastic properties of dentin. Aging, systemic conditions like diabetes, and external treatments such as irradiation can weaken the dentin and make teeth more prone to vertical root fractures (VRF). Moreover, environmental and ethnic variations affect dentin’s microstructure and mechanical properties, complicating a one-size-fits-all approach to endodontic treatment [5, 6, 7, 8]. Thus, it is important to realize that there are physiological (non-iatrogenic) and iatrogenic factors (endodontic treatment procedures) that can alter the mechanical characteristics of dentin.
Biomechanics and Tooth Function
A tooth is a dynamic structure that responds to masticatory stresses and thermal changes. Stress and strain distribution patterns vary across teeth, while it is established that stress induced by chewing is predominantly distributed in the cervical region of the root. However, the nature of stress distribution in a tooth is influenced by tooth anatomy, contacts with adjacent teeth, and support from alveolar bone [5, 9]. Endodontically treated teeth exhibit altered biomechanical behavior due to the loss of intra-pulpal hydrostatic pressure and subsequent loss of free water in dentin, regardless of the size or shape of the access cavity. This underlines the importance of preserving cervical root dentin or peri-cervical dentin (PCD), which is crucial in transferring functional stresses and ensuring long-term survival.
Does Minimally Invasive Endodontics Enhance Tooth Strength?
Traditional endodontic access cavities are associated with increased cuspal flexure and higher concentrations of stress and strain, which can make teeth more susceptible to fractures. Contracted endodontic cavities (CECs) aim to preserve dentin and reduce overall stress, but in vitro studies have yielded mixed results regarding whether this consistently improves fracture resistance, particularly when bonded restorations are used. A review of the literature suggests that while preserving coronal tooth structure and PCD is generally beneficial, the evidence remains divided on whether this translates into significantly enhanced fracture strength [10-15]. Most studies concur that dentin conservation reduces the risk of catastrophic tooth failure. However, the impact of minimally invasive techniques on the fracture resistance of teeth restored with bonded composite resins or onlays remains inconclusive [16-18]. Additionally, increased apical enlargement and taper during canal instrumentation have been consistently linked to reduced root strength, especially in anatomically complex regions such as isthmuses and middle mesial canals, where fracture risk is elevated [19-21]. These findings suggest that, beyond access cavity design, the size and taper of canal instrumentation are critical factors in root biomechanics. In many cases, smaller and more conservative preparations may offer mechanical advantages without compromising disinfection efficacy.
Restoration: Critical to Long-Term Success
Preserving the dentin located around the cervical area of the root or PCD is a central goal in minimally invasive endodontics due to its critical role in maintaining tooth strength and structural integrity. Several strategies have been proposed to restore or preserve this important zone. These strategies include the use of flowable composites and giomers to bond and reinforce PCD, as well as conservative access cavity designs that preserve marginal ridges and maintain the tooth’s inherent structural integrity.
The type and timing of restoration are critical factors in the long-term survival of endodontically treated teeth. Molars without full cuspal coverage have significantly lower survival rates in a 10-year retrospective study. Presence of crowns resulted in 91% survival rate compared to direct restorations (76%) [22]. Restorative options for endodontically treated teeth include both direct and indirect approaches, each with distinct advantages and limitations. Direct bonded composite resins are conservative but sensitive to polymerization shrinkage and the C-Factor, and their success depends heavily on the quality of the remaining dentin. Indirect adhesive restorations, such as onlays, offer improved strength and aesthetics while still preserving tooth structure. Importantly, restorations that provide full cuspal coverage, incorporating a 2 mm ferrule and well-designed occlusal contacts, significantly enhance the tooth’s biomechanical resilience and longevity. While short-term survival rates for indirect restorations are promising, long-term outcomes are strongly influenced by factors such as residual dentin quality, occlusal forces, and the effectiveness of bonding techniques [23].
Disinfection: A Compromised Trade-Off?
Minimally invasive access and instrumentation techniques, while advantageous for preserving tooth structure, may compromise the efficacy of root canal disinfection, particularly in complex canal anatomies and the apical third [24-26]. The conventional syringe-needle irrigation method with antimicrobial agents remains the clinical standard, yet its effectiveness is limited by its inability to adequately reach and disinfect the entire root canal system [25]. Furthermore, the correlation between bacterial load reduction and clinical healing outcomes remains unclear, especially in cases where conservative approaches are used. To overcome these limitations, emerging technologies are being explored to enhance antimicrobial efficacy within minimally prepared canals.
Redefining Minimally Invasive Endodontics
Minimally invasive dentistry involves more than just conservative cavity preparation and dentin preservation; it also emphasizes patient education, caries prevention, early detection, and timely intervention [27]. In the context of endodontics, a minimally invasive approach extends beyond carefully designed access cavities and conservative shaping of the root canal system. It involves a broader perspective that includes accurate diagnosis and an understanding of the etiological and biological factors influencing disease progression to guide appropriate treatment decisions [28]. This paradigm includes the early identification of pulpitis and the implementation of conservative therapeutic measures such as vital pulp therapy, aimed at preventing the need for root canal treatment. In persistent lesions with failing primary treatment, alternative treatments like root-end microsurgery or tooth replantation may offer more conservative and biologically sound solutions compared to re-instrumentation of the root canal system. Ultimately, minimally invasive endodontics aims to preserve the natural tooth structure while effectively managing disease and maintaining long-term oral health.
Next-Gen Innovations: The Role of Nanotechnology and Tissue Engineering
A pivotal insight from the presentation was the recognition that periapical healing depends on more than just bacterial elimination; it is also shaped by the interactions between microbial communities and the host immune system. This reflects a paradigm shift from a purely antimicrobial approach to one that incorporates immunomodulation as a fundamental component of healing. Key findings indicate that prolonged inflammation can significantly hinder tissue repair, whereas targeted modulation of the immune response may facilitate the transition from a diseased state to regeneration by balancing pro- and anti-inflammatory signals.
To address the biomechanical deficiencies in dentin caused by dehydration and aging, researchers are developing advanced biomaterials that not only reinforce tooth structure but also promote healing. Among these innovations, bioactive and functionalized nanoparticles have shown considerable promise. These nanoparticles can disrupt bacterial biofilms, inducing collagen cross-linking within the dentin extracellular matrix – a process known as microtissue engineering [29] and modulating immune responses to enhance tissue repair [30]. By guiding cellular behavior to reduce inflammation and support organized regeneration, bioactive engineered nanoparticles significantly expand the regenerative potential of endodontic therapy. The integration of both antibacterial and immunomodulatory properties in these materials represents a major advancement in minimally invasive endodontics, offering the potential for improved mechanical durability and superior clinical outcomes in endodontically treated teeth.
In conclusion, minimally invasive endodontics is not a one-size-fits-all solution but rather a dynamic concept requiring careful balance between conservation, disinfection, and restoration. The future of endodontics lies not just in doing less, but in doing optimized preservation of dentin while enhancing its strength, ensuring effective microbial control, and harnessing the host immune machinery for optimal healing. With continued innovation and evidence-based refinement, minimally invasive endodontics holds the potential to significantly elevate both functional outcomes and patient satisfaction in modern endodontics.
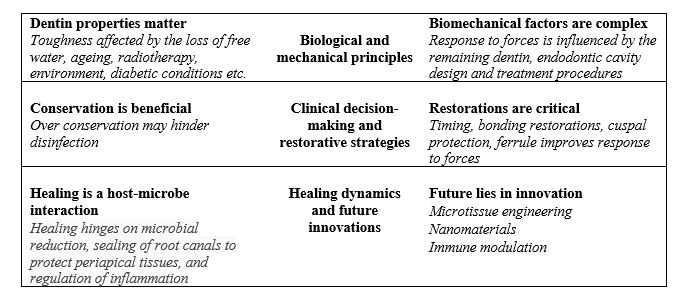
Figure 1: Summary showing the highlights and takeaways.

Figure 2: Sequential radiographs highlight the role of mechanical preparation and biological disinfection in achieving and maintaining periapical health.
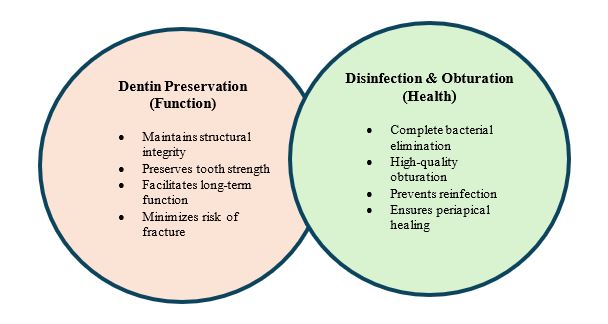
Figure 3: Diagram emphasizing the balance between dentin preservation (function) and disinfection with obturation (health) in endodontic treatment. Preservation must not compromise disease control.
References
- Lui S, Zhou J. Comparative efficacy and safety of three surgical procedures for the treatment of lumbar disc herniation: a Baysian-based network analysis. BMC Surgery. 2025 25:125
- Flaifel M, Eichenberg S, Mohandes B, Taha E, Kollman L, Flemming S, et.al. The outcomes of robotic ileocolic resection in Crohn’s disease compared with laparoscopic and open surgery: a meta-analysis and systematic review. Techniques in Coloproctology 2025 March 29:88
- Jameson MW, Hood JA, Tidmarsh BG. The effects of dehydration and on some mechanical properties of human dentine. J Biomech 1993; 26:1055–65.
- Kishen A. Vedantam A. Hydromechanics in dentine: Role of dentinal tubules and hydrostatic pressure on mechanical stress-strain distribution. Dental Materials. 2007;23(10):1296-306.
- Kishen A. Mechanisms and risk factors for fractures in endodontically treated teeth. Endodontic topics 2006;13:57-83;
- PradeepKumar AR, JothiLatha S, Durvasulu A, Muralidhar L, Vimalesh Alagu J, Shereen J,Kishen A. Impact of Type 2 Diabetes Mellitus on the Occurrence of Vertical Root Fracture: A Case Control Study. J Endod 2024 Jan 24:S0099-2399(24)00039-6;
- Ivancik, Dwayne D Arola. The importance of microstructural variations on the fracture toughness of human dentin. Biomaterials 2013 Jan;34(4):864-74;
- Celik Dursun P, Sengul F, Yilmaz Y, Sezen O. Effects of irradiation, restoration and crown fracture type on the maximum load to fracture traumatized incisors: An ex vivo study. Dent Traumatol. 2022 Oct;38(5):417-423.
- Asundi A, Kishen A. In vivo strain and in vitro stress distribution in dental supporting structures- a strain gauge and photoelastic analysis. Archives of Oral Biology 2000; 45:543-50).
- Plotino G, Grande NM, Isufi A, Ioppolo P, Pedullà E, Bedini R, Gambarini G, Testarelli L. Fracture Strength of Endodontically Treated Teeth with Different Access Cavity Designs.
J Endod. 2017 Jun;43(6):995-1000.
- Peng W, Zhou X, Gao Y, Xu X. Effect of Access Cavity Preparation on Dentin Preservation, Biomechanical Property, and Instrumentation Efficacy: A Micro-Computed Tomographic Study. J Endod. 2022 May;48(5):659-668.
- Vorster M, van der Vyver PJ, Markou G. The Effect of Different Access Cavity Designs in Combination with WaveOne Gold and TruNatomy Instrumentation on Remaining Dentin Thickness and Volume. J Endod. 2023 Jan;49(1):83-88
- Meyerson D, Li FC, Kishen A. Photomechanical investigation on the impact of endodontic cavity design on the biomechanical response in mandibular posterior teeth. J Endod 2025 Jan;51(1):78-84.
- Abou-Elnaga MY, Alkhawas MAM, Kim HC, Refai AS. Effect of Truss Access and Artificial Truss Restoration on the Fracture Resistance of Endodontically Treated Mandibular First Molars. J Endod. 2019 Jun;45(6):813-817.
- Krishan R, Paqué F, Ossareh A, Kishen A, Dao T, Friedman S. Impacts of conservative endodontic cavity on root canal instrumentation efficacy and resistance to fracture assessed in incisors, premolars, and molars. J Endod. 2014 Aug;40(8):1160-6.
- Selvakumar RJ, Surendran S, Sundar S, Arul B, Natanasabapathy V. Impact of Contracted Endodontic Access Cavities on the Fracture Resistance of Endodontically Treated Teeth After Mechanical Aging by Simulated Chewing Forces. J Endod. 2023 Sep;49(9):1176-1182.
- Daniel A, Saleh AR, Al-Jadaa A, Kheder W. Impact of Access Cavity Design on Fracture Resistance of Endodontically Treated Maxillary First Premolar: In Vitro. Braz Dent J. 2024 Mar 22;35:e245676.
- Moore B, Verdelis K, Kishen A, Dao T, Friedman S Impacts of Contracted Endodontic Cavities on Instrumentation Efficacy and Biomechanical Responses in Maxillary Molars. J Endod. 2016 Dec;42(12):1779-1783.
- Keleş A, Keskin C, Karataşlıoğlu E, Kishen A, Versiani MA. Middle Mesial Canal Preparation Enhances the Risk of Fracture in Mesial Root of Mandibular Molars. J Endod. 2020 Sep;46(9):1323-1329.
- Sabeti M, Kazem M, Dianat O, Bahrololumi N, Beglou A, Rahimipour K, Dehnavi F. Impact of Access Cavity Design and Root Canal Taper on Fracture Resistance of Endodontically Treated Teeth: An Ex Vivo Investigation. J Endod. 2018 Sep;44(9):1402-1406.
- von Arx T, Bosshardt D. Vertical root fractures of endodontically treated posterior teeth: A histologic analysis with clinical and radiographic correlates. Swiss Dent J. 2017 Jan 12;127(1):14-23.
- Landys Boren, D., Jonasson, P.& Kvist, T. Long-term survival of endodontically treated teeth at a public dental specialist clinic. J Endod 2015, 41, 176–181.
- Dioguardi M, Alovisi M, Troiano G, Caponio CVA, Baldi A, Rocca GT, Comba A, Lo Muzio L, Scotti N. Clinical outcome of bonded partial indirect posterior restorations on vital and non-vital teeth: a systematic review and meta-analysis. Clin Oral Investig. 2021 Dec;25(12):6597-6621.
- Neelakantan P, Khan K, Hei Ng GP, Yip CY, Zhang C, Pan Cheung GS. Does the Orifice-directed Dentin Conservation Access Design Debride Pulp Chamber and Mesial Root Canal Systems of Mandibular Molars Similar to a Traditional Access Design? J Endod. 2018 Feb;44(2):274-279. doi: 10.1016/j.joen.2017.10.010. Epub 2017 Dec 19. PMID: 29273493.
- Rover G, Belladonna FG, Bortoluzzi EA, De-Deus G, Silva EJNL, Teixeira CS. Influence of Access Cavity Design on Root Canal Detection, Instrumentation Efficacy, and Fracture Resistance Assessed in Maxillary Molars. J Endod. 2017 Oct;43(10):1657-1662. doi: 10.1016/j.joen.2017.05.006. Epub 2017 Jul 21. PMID: 28739013.
- Boutsioukis, C.& Arias-Moliz, M.T. (2022) Present status and future directions – irrigants and irrigation methods. International Endodontic Journal, 55(Suppl. 3), 588–
- Murdoch-Kinch CA, McLean ME. Minimally invasive dentistry. J Am Dent Assoc. 2003 Jan;134(1):87-95. doi: 10.14219/jada.archive.2003.0021. PMID: 12555961.
- Gutmann JL. Minimally invasive dentistry (Endodontics). J Conserv Dent. 2013 Jul;16(4):282-3. doi: 10.4103/0972-0707.114342. PMID: 23956526; PMCID: PMC3740635.
- . Li FC, Nicholson E, Singh CV, Kishen A. Microtissue Engineering Root Dentin with Photodynamically Cross-linked Nanoparticles Improves Fatigue Resistance of Endodontically Treated TeethJ Endod. 2020 May;46(5):668-674
- Hussein H, Kishen A. Proteomic profiling reveals engineered chitosan nanoparticles mediated cellular crosstalk and immunomodulation for therapeutic application in apical periodontitis. Bioact Mater. 2021 Oct 9;11:77-89.
