Can Calcium Silicate-Based Sealer Cases Be Retreated?
By Ji Wook Jeong, DMD, MSD
Since Larry Hench described the potential use of silica in medicine in 1971 due to its biocompatibility, a variety of silicate-based materials have been introduced in biomedical engineering. For over 30 years, mineral trioxide aggregate has been used in dentistry for a variety of specialized treatments including repairing perforation, performing endodontic surgery, and capping pulps to help save teeth. The popularity of calcium silicate-based sealers (CSS) among clinicians has steadily grown since the introduction of iRoot SP (Innovative Biocermix) in 2007. However, two contradictory questions about CSS have emerged among clinicians: “Does CSS set completely?” and “Can CSS be retreatable?”
Several clinical studies have addressed the question of whether CSS set completely. If it does not set completely, the concern shifts from retreatability to potential for poor outcomes. A 2018 retrospective study from Texas A&M University with a 30.1-month follow-up observed a 91% success rate when using EndoSequence CSS, suggesting that sealer extrusion does not negatively impact outcomes (1). Similarly, a non-randomized clinical study from Guy’s and St. Thomas’s Foundation, London, UK, with a 12-month recall period, demonstrated that BioRoot RCS CSS produced comparable results (84% success rate) to AH Plus sealer (80% success rate) which is considered the gold standard epoxy resin-based sealer (2). Additionally, a randomized controlled clinical trial from Yonsei University, Seoul, South Korea, found that the success rate of sealer-based obturation techniques using Endoseal TCA was higher than continuous wave condensation using AH Plus sealer, although the difference was not statistically significant (3). These studies collectively indicate that CSS does set sufficiently and its setting behavior is not a major concern for clinical success. Of course, if CSS is not used properly, such as by applying it to the root canals that are too wet due to the presence of pus or exudates, it may not set properly, leading to leakage and the need for retreatment.
In 1958, Grossman proposed the ideal qualities of root canal sealers, including tackiness, hermetic sealing, radiopacity, ease of mixing, minimal shrinkage upon setting, hard set in the canals, no tooth staining, bacteriostatic properties, slow setting, insolubility in tissue fluids, tissue tolerance, and solubility during retreatment (4). However, this last suggestion of solubility during retreatment remains a controversial issue with CSS. While some clinicians report difficulty penetrating CSS during the removal of root canal fillings, describing it as “concrete-like,” others have not encountered any problems.
According to a survey study (5), for the question, “Do you think BioCeramic Root canal sealer usage may influence the ability to re-establish apical patency during non-surgical retreatment?”, 68% of general dentists expressed concern about apical patency. It’s interesting to note that 52% of endodontists also shared this concern, even though they have received training in retreatment procedure. This raises the question of why some endodontists still have worries about re-establishing apical patency despite their specialized training. It’s possible that some endodontists may have more experience or training in retreatment than others, which could affect their confidence levels in achieving apical patency. However, they may have a limited number of cases sealed with calcium silicate-based sealers so far, leading to positive or negative assumptions based on a small sample size. Furthermore, factors such as the complexity of the cases, canal anatomy, and other variables may contribute to varying levels of concerns about apical patency among endodontists.
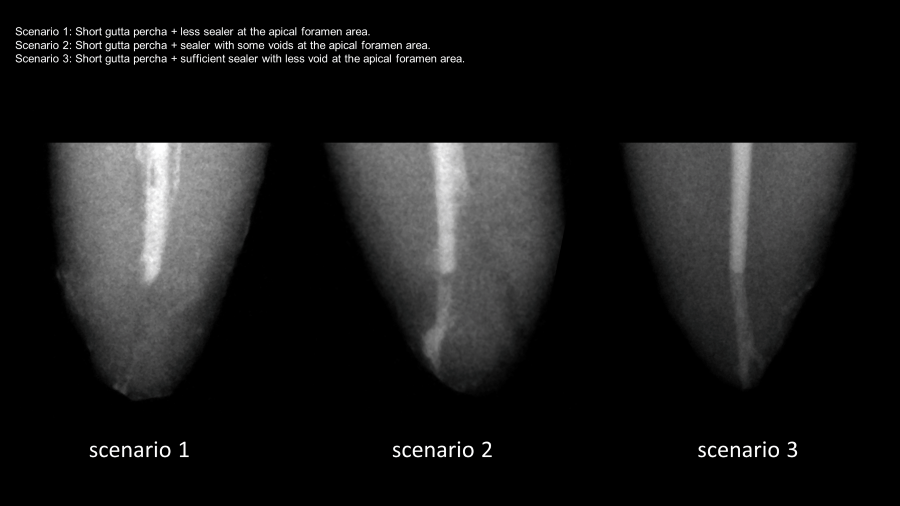
Although strategies for retreatment of CSS-filled canals should require minimal changes, some clinicians express concerns about re-establishing apical patency when gutta-percha is placed short of the working length. This concern is supported by studies like the one by Hess et al. which reported a 30% patency rate in such cases (6). Additionally, the lack of definitive solvents for CSS adds to the complexity of the process. However, a recent ex-vivo study found that using a solvent, 10% formic acid achieved a 100% patency rate, although it did not demonstrate statistically significant differences in efficacy compared to chloroform (93%) (7). The observed fluctuations in retrieval rates likely arise from variations in the samples themselves, rather than from differences in the solvents or techniques employed, as demonstrated in Figures. This highlights the importance of standardizing sample design in research on this topic.
In addition to standardizing the sample design, it’s crucial to classify CSS based on its setting properties, ranging from soft set to hard set. This is because different brands of CSS exhibit varying degrees of retrievability, with softer set materials generally allowing for easier removal (8).
Research on the retrievability of CSS is still in its early stages, with limited clinical data available. Therefore, it’s too early to say for sure how easy it is to remove CSS and dentists must carefully weigh the benefits and risks for each patient before making decision on retreatment options and strategies.
- Chybowski EA, Glickman GN, Patel Y, Fleury A, Solomon E, He J. Clinical Outcome of Non-Surgical Root Canal Treatment Using a Single-cone Technique with Endosequence Bioceramic Sealer: A Retrospective Analysis. J Endod 2018;44(6):941-945.
- Zavattini A, Knight A, Foschi F, Mannocci F. Outcome of Root Canal Treatments Using a New Calcium Silicate Root Canal Sealer: A Non-Randomized Clinical Trial. J Clin Med 2020;9(3).
- Kim JH, Cho SY, Choi Y, Kim DH, Shin SJ, Jung IY. Clinical Efficacy of Sealer-based Obturation Using Calcium Silicate Sealers: A Randomized Clinical Trial. J Endod 2022;48(2):144-151.
- Grossman LI. An improved root canal cement. J Am Dent Assoc 1958;56(3):381-385.
- Guivarc’h M, Jeanneau C, Giraud T, Pommel L, About I, Azim AA, et al. An international survey on the use of calcium silicate-based sealers in non-surgical endodontic treatment. Clin Oral Investig 2020;24(1):417-424.
- Hess D, Solomon E, Spears R, He J. Retreatability of a bioceramic root canal sealing material. J Endod 2011;37(11):1547-1549.
- Rezaei G, Liu X, Jalali P. Efficacy of Different Solvents for Achieving Patency in Teeth Obturated Using Bioceramic Sealer. J Endod 2023;49(2):219-223.
- Carrillo CA, Kirkpatrick T, Freeman K, Makins SR, Aldabbagh M, Jeong JW. Retrievability of Calcium Silicate-based Root Canal Sealers During Retreatment: An Ex Vivo Study. J Endod 2022;48(6):781-786.
Dr. Ji Wook Jeong is assistant professor/research director/Endodontics at UT Health School of Dentistry.




