Regenerative Endodontic Therapy: A Treatment With Substantial Benefits
By Vanessa Chrepa, D.D.S., M.S., assistant professor, University of Washington School of Dentistry
Regenerative endodontics is one of the most remarkable advancements in our specialty. The idea that one can replace damaged structures and regain functionality (such as nociception and immune competency) in previously necrotic and infected root canal systems has been groundbreaking. Since the introduction of regenerative pulp therapy as a viable treatment in the early 2000s, endodontists and other scientists have continued to discover its crucial benefit to immature teeth and its capacity to overcome the limitations of conventional root canal treatment. Utilizing regenerative endodontic therapy aids endodontists in our ultimate goal of helping our patients retain their natural dentition.
Teeth with incomplete root development have short roots with thin walls, which compromises their longevity. Through regenerative therapy, we can facilitate root development in previously immature teeth with necrotic pulps. This is a significant benefit over conventional root canal treatment and especially valuable for young patients, as teeth preservation is critical to their skeletal and dental development.
Regenerative endodontic protocol provides clinicians with a relatively standardized procedure in an effort to achieve more predictable outcomes. This protocol has undergone significant changes since it was first introduced by Banchs and Trope in 2004.1 Following the discovery that regenerative endodontics is a stem cell-based treatment2 it was determined that a more "guided" tissue engineering approach is necessary in order to reproduce the original pulp tissue morphology and function. Consequently, subsequent protocols have been modified to be more "stem cell-friendly" by advocating a disinfection protocol that promotes stem cell survival and proliferation followed by restoration with biocompatible materials. The current AAE-recommended regenerative endodontic protocol includes the use of 1.5% sodium hypochlorite (NaOCl) instead of 6% NaOCl, dilution of the double or triple antibiotic paste (TAP) to 0.1-1 mg/ml and final canal rinse with EDTA prior to induction of periapical bleeding.
Regenerative endodontic procedures are highly successful. When compared with MTA apexification, studies have reported similar success and survival rates for regenerative endodontics, in the range of 90-100%. Although clinical cases with longer follow-ups are limited, they have reported favorable outcomes.3 In addition to resolution of clinical signs and symptoms and periapical healing, regenerative endodontic procedures have shown approximately 15% increase in root length and 29% increase in root width that was very significant compared to apexification procedures.4 This substantial increase in root development is a crucial benefit as it may have a positive effect on the longevity of the immature tooth. These advantages are unparalleled with any other endodontic treatment.
In addition, many researchers have begun to apply regenerative endodontic procedures to mature teeth in adult patients. Several clinical case reports have shown complete resolution of signs and symptoms of pulp necrosis in mature teeth, even those with large periapical lesions, as well as signs of pulp canal obliteration.5, 6 A study in 2011 demonstrated for the first time that inflamed periapical tissues are a significant source of mesenchymal stem cells (MSCs) in adult patients and mature teeth.7 Following that discovery, my former colleagues at the University of Texas Health Science Center at San Antonio and I performed a clinical trial to assess the ability to transfer MSCs by evoking bleeding in mature teeth with apical lesions in adults.8 Indeed, evoked bleeding from the periapical tissues led to a significant influx of MSCs into root canal systems of mature teeth in adults that was comparable to the clinical delivery of MSCs demonstrated before in immature teeth. These cells also expressed genes related to stem cell homing, angiogenesis and odontoblastic differentiation - all critical components to dental pulp regeneration. Therefore, clinical delivery of MSCs in root canals of mature teeth is feasible. This discovery may provide the basis for future applications of regenerative endodontic therapy in fully formed teeth in adults.
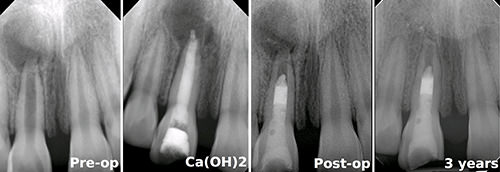 |
| Twelve-year-old female presented with complicated crown fracture on tooth #8 due to a previous traumatic injury. Diagnosis of #8 was pulp necrosis with symptomatic apical periodontitis. Regenerative endodontic treatment was elected and treatment was performed in two visits with calcium hydroxide [Ca(OH)2] as interim medicament. Canal was irrigated with 1.5% NaOCl and 17% EDTA following the AAE's recommended protocol. MTA barrier was placed below the CEJ to minimize discoloration and tooth was restored with glass ionomer and composite restoration. Three-year follow-up shows complete periapical healing and continuation of root development. Note that the treatment was successful even in the presence of a large cystic-like periapical lesion. Images courtesy of Dr. Vanessa Chrepa. |
Though the clinical results have been favorable and the research advancements very promising, regenerative endodontic therapy does have some limitations:
- The treatment itself is very technique-sensitive and requires substantial training; evoking bleeding and placement of the biomaterial over an unstable blood clot can be challenging. For a trained clinician, however, the procedure may be more time-effective than an MTA apexification. Obturation of the apical third of an immature tooth can sometimes be more tedious and time-consuming than obturating the coronal third.
- Tooth discoloration is very common either due to the minocycline in the TAP or the MTA barrier placed at the cemento-enamel junction (CEJ). This appears to be the primary concern for most patients at recall appointments. Discoloration can be minimized, though,
through the use of double antibiotic paste (i.e., metronidazole and ciprofloxacin)
or calcium hydroxide as an inter-appointment dressing alternative and by using other biocompatible materials, such as Biodentiner, as a barrier. - If post placement is required, regenerative endodontic procedures do not provide adequate space as the MTA barrier is placed at the CEJ level. In order to achieve the best of both worlds, one could consider regenerative endodontic treatment in order to achieve further root development and apical closure, followed by root canal treatment and post placement.
Despite these limitations, regenerative endodontic therapy has the potential to redefine endodontic treatment. Vital teeth have been shown to be less susceptible to caries than root canal-treated teeth, and with regenerative endodontic therapy, a viable neurovascular tissue with defense mechanisms occupies the root canal system instead of a rubber material. This treatment gives teeth the chance to regain their vitality and sensibility and improve their function. We can save more teeth and positively impact more patients' lives!
For more AAE resources on regenerative endodontics, visit aae.org/regenerativeendo.
 |
 |
|
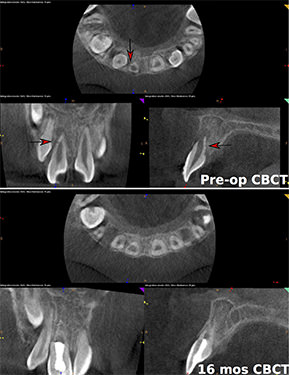
| Nine-year-old male presented with history of avulsion of tooth #8 three months prior to dental visit. Patient's parent reported that their dentist replanted tooth #8 within two hours of the accident. Diagnosis of #8 was pulp necrosis with symptomatic apical periodontitis. Preoperative cone beam computed tomography was made prior to treatment and external inflammatory root resorption was noted (see arrows). Regenerative endodontic treatment was elected and treatment was performed in two visits with calcium hydroxide [Ca(OH)2] as interim medicament. Canal was irrigated following AAE's recommended protocol. MTA barrier was placed below the CEJ to minimize discoloration and tooth was restored with glass ionomer and composite restoration. Sixteen-month follow-up shows complete periapical healing and continuation of root development. No sign of root resorption was noted at the follow-up visit. Images courtesy of Dr. Vanessa Chrepa. | ||
Dr. Vanessa Chrepa is an assistant professor in the Department of Endodontics at the University of Washington School of Dentistry. She is a Diplomate of the American Board of Endodontics and accomplished researcher in the field of regenerative endodontics. She can be reached at chrepa@uw.edu.
References:
- Banchs F, Trope M. Revascularization of immature permanent teeth with apical periodontitis: new treatment protocol? J Endod 2004;30:196-200.
- Lovelace TW, Henry MA, Hargreaves KM, Diogenes A. Evaluation of the delivery of mesenchymal stem cells into the root canal space of necrotic immature teeth after clinical regenerative endodontic procedure. J Endod 2011;37:133-8.
- Diogenes A, Ruparel NB, Shiloah Y, Hargreaves KM. Regenerative endodontics: a way forward. J Am Dent Assoc 2016;147:372-80.
- Jeeruphan T, Jantarat J, Yanpiset K, Suwannapan L, Khewsawai P, Hargreaves KM. Mahidol study 1: comparison of radiographic and survival outcomes of immature teeth treated with either regenerative endodontic or apexification methods: a retrospective study. J Endod 2012;38:1330-6.
- Saoud TM, Sigurdsson A, Rosenberg PA, Lin LM, Ricucci D. Treatment of a large cystlike inflammatory periapical lesion associated with mature necrotic teeth using regenerative endodontic therapy. J Endod 2014;40:2081-6.
- Paryani K, Kim SG. Regenerative endodontic treatment of permanent teeth after completion of root development: a report of 2 cases. J Endod 2013;39:929-34.
- Liao J, Al Shahrani M, Al-Habib M, Tanaka T, Huang GT. Cells isolated from inflamed periapical tissue express mesenchymal stem cell markers and are highly osteogenic. J Endod 2011;37:1217-24.
- Chrepa V, Henry MA, Daniel BJ, Diogenes A. Delivery of apical mesenchymal stem cells into root canals of mature teeth. J Dent Res 2015;94:1653-9.




