Cracked Teeth: To Treat or Not to Treat?

By Suhaila S. Shariff D.M.D., M.P.H. and Matthew C. Davis D.D.S.
From an endodontist’s perspective, assessing the prognosis while managing cracked teeth is a challenge due to varying degrees of crack progression along the longitudinal axis of the tooth. There is a research-based consensus that the outcomes of endodontically treated cracked teeth, where a crack is confined to the clinical crown, are favorable as long as a full coverage coronal restoration is placed1–4. Historically, there has been non-evidence-based conjecture that teeth with deeper cracks extending onto the root surface internally and encroaching on the periodontium externally (i.e., a radicular extension) have a poor prognosis and should therefore be extracted. However, newer studies involving datasets or subsets of deeply cracked teeth are reporting more favorable outcomes demonstrating survival rates ranging from 82-96% and up to 91% success5–8. Collectively, these studies indicate that cracked teeth, even those with radicular extension, may carry a favorable prognosis.
What sets deeply cracked teeth apart from their intact, non-cracked counterparts is the presence of a crack originating in the clinical crown and extending along the radicular structures, often entering the orifice of the canal. A deeper crack potentially weakens the tooth9 and root and can serve as an area of continued bacterial ingress10. Theoretically, in these cases, it would seem that we should alter our endodontic treatment techniques to address the microleakage and weakened tooth structure in the vulnerable cervical area. This idea prompted us to design and perform a prospective study looking at success and survival in cracked teeth with radicular extensions utilizing an altered endodontic treatment protocol specific for deep cracks. As a result of this modified protocol, we saw upwards of 90% success and 96% survival rates over 2–4 years following endodontic treatment5. These outcomes are similar to success and survival rates in studies of non-cracked endodontically treated teeth11–13. Table 1 outlines the modifications employed in our study:
| Table 1: Cracked Teeth Treatment Modifiers (Davis & Shariff 2019)5 | |
| Intra-Operative | Intraradicular Barriers (Deep Orifice Plugs) |
| Post-Operative | Take the tooth entirely out of occlusion immediately following RCT
Patient Education: Avoid chewing on the affected tooth side until crown restoration is completed Expeditious Crown Placement |
| Follow-Up: 6 weeks | Verify Crown Restoration
Check Occlusion |
The first treatment modifier utilized in our study was post-obturation microscope-assisted intraorifice barriers placed 2-3mm apical to the crack’s extent (Figure 1). The ubiquitous presence of bacteria in cracks has been documented histologically10. This bacterial load in the deep crack could result in a continual source of contamination risking subsequent endodontic disease. Many studies have demonstrated improved coronal leakage control with orifice barriers14; therefore, sealing the crack below its apical extent could mitigate the risk of future infection. As an additional benefit, orifice plugs have also been shown to increase fracture resistance at the cervical level15,16 conferring an obvious benefit to these cracked teeth.
Another crucial modification in this study was that every tooth was required to have a full-coverage crown immediately following endodontic treatment. Many studies established the importance of crown placement for success and survival of endodontically treated teeth in general1,13. A crown is even more essential for cracked teeth. One study showed a 2-year survival rate of only 20% when endodontically treated cracked teeth were restored without a crown versus 94% survival for those that were crowned2. Another landmark study noted that following a crown restoration, signs of crack propagation were noted in only 4% of cracked teeth17. Additionally, timing on crown placement is imperative as modern studies have shown a significant increase in favorable outcomes for cracked teeth when they are restored expeditiously following endodontic treatment3–5,18. Delaying the coronal restoration poses significant risk of crack propagation, split tooth, and failure.
Other important modifiers in the study included: adjusting the tooth out of occlusion immediately following endodontic treatment, instructing the patient not to chew on the affected side until after crown restoration, and scheduling follow-up appointments to check and adjust occlusion as necessary. Occlusal discrepancies likely have a profound impact on the success of endodontic procedures. Malocclusion (hyperocclusion or excursive interferences) and parafunction, in one study, showed a significantly higher association with the presence of fractures in teeth19. In our study, 79% of returning patients required occlusal adjustment of their new crown, demonstrating the importance of follow-up appointments to ensure proper occlusion5.
Along with these treatment modifiers, it is also important to employ current endodontic techniques and imaging when managing deeply cracked teeth. Microscopes, conservative canal preparations, and aseptic techniques are as important to achieving endodontic success in this subset as it is in all endodontic cases. The role of cone-beam computed tomography (CBCT) in diagnosis is invaluable, as a pre-operative scan can demonstrate narrow periodontal defects directly adjacent to cracks at the crestal bone level, showcasing the presence of a radicular crack20 (Figure 1). This crack-associated isolated periodontal pocketing or CAIPP, due to its size and interproximal location, often eludes periodontal probing. Our study, now in the tenth year of data collection, shows the majority of cracked teeth with radicular extension continue to display this CAIPP defect on follow-up CBCT imaging but typically show little to no change over time (Figure 2). These teeth have remained asymptomatic and functional. From this it can be concluded that a CAIPP should not dissuade practitioners from performing endodontic treatment. As with non-cracked teeth, condemning a cracked tooth based on a small, isolated pocket does not seem justified.
So, we are left with the question: which deeply cracked teeth should be treated and which ones should not? Until future evidence suggests otherwise, it is recommended that case selection parameters include: 1) no clinical or radiographic signs of a split tooth (complete fracture); 2) the crack should not extend across the floor of the pulp chamber7; and 3) the internal extent of the crack should be visible microscopically to ensure placement of the intraradicular barrier apical to it5. If these conditions are not met, then according to present evidence, the prognosis becomes questionable or poor, and extraction may need to be considered.
In conclusion, newer independent studies are demonstrating outcomes for endodontically treated cracked teeth with radicular extensions to be similar to their non-cracked counterparts. While none of our procedures come with guaranteed success, modern endodontic techniques, case selection parameters, and treatment modifiers are allowing us to predictably save more cracked teeth. We know that patients wish to preserve their natural dentition, and they look to us to achieve this goal. We ought to consider extraction an inferior alternative to saving cracked teeth. After all, saving teeth is what we endodontists do.
REFERENCES
- Aquilino, S. A. & Caplan, D. J. Relationship between crown placement and the survival of endodontically treated teeth. Journal of Prosthetic Dentistry 87, 256–263 (2002).
- Chen, Y. T., Hsu, T. Y., Liu, H. & Chogle, S. Factors Related to the Outcomes of Cracked Teeth after Endodontic Treatment. J Endod 47, 215–220 (2021).
- Nguyen Thi, W. & Jansson, L. Survival rate after endodontic treatment in general dentistry for cracked teeth with different coronal restorations. Acta Odontol Scand 79, 256–261 (2021).
- de Toubes, K. M. S. et al. The Correlation of Crack Lines and Definitive Restorations with the Survival and Success Rates of Cracked Teeth: A Long-term Retrospective Clinical Study. J Endod 48, 190–199 (2022).
- Davis, M. C. & Shariff, S. S. Success and Survival of Endodontically Treated Cracked Teeth with Radicular Extensions: A 2- to 4-year Prospective Cohort. J Endod 45, 848–855 (2019).
- Kang, S. H., Kim, B. S. & Kim, Y. Cracked teeth: Distribution, characteristics, and survival after root canal treatment. J Endod 42, 557–562 (2016).
- Sim, I. G., Lim, T. S., Krishnaswamy, G. & Chen, N. N. Decision Making for Retention of Endodontically Treated Posterior Cracked Teeth: A 5-year Follow-up Study. J Endod 42, 225–229 (2016).
- Leong, D. J. X., de Souza, N. N., Sultana, R. & Yap, A. U. Outcomes of endodontically treated cracked teeth: a systematic review and meta-analysis. Clin Oral Investig 24, 465–473 (2020).
- Kishen, A. & Asundi, A. Photomechanical investigations on post endodontically rehabilitated teeth. J Biomed Opt 7, 262 (2002).
- Ricucci, D., Siqueira, J. F., Loghin, S. & Berman, L. H. The cracked tooth: Histopathologic and histobacteriologic aspects. J Endod 41, 343–352 (2015).
- Ng, Y.-L., Mann, V., Rahbaran, S., Lewsey, J. & Gulabivala, K. Outcome of primary root canal treatment: systematic review of the literature – part 1. Effects of study characteristics on probability of success. Int Endod J 40, 921–39 (2007).
- Burns, L. E. et al. Outcomes of primary root canal therapy: An updated systematic review of longitudinal clinical studies published between 2003 and 2020. International Endodontic Journal vol. 55 714–731 Preprint at https://doi.org/10.1111/iej.13736 (2022).
- Ng, Y.-L., Mann, V. & Gulabivala, K. Tooth survival following non-surgical root canal treatment: a systematic review of the literature. Int Endod J 43, 171–89 (2010).
- Pisano, D. M., DiFiore, P. M., McClanahan, S. B., Lautenschlager, E. P. & Duncan, J. L. Intraorifice sealing of gutta-percha obturated root canals to prevent coronal microleakage. J Endod 24, 659–662 (1998).
- Chauhan, P., Garg, A., Mittal, R. & Kumar, H. A comparative evaluation of fracture resistance of endodontically treated teeth using four different intraorifice barriers: An in vitro study. Journal of Conservative Dentistry 22, 420 (2019).
- Boonrawd, N., Rungsiyakull, P., Rungsiyakull, C. & Louwakul, P. Effects of composite resin core level and periodontal pocket depth on crack propagation in endodontically treated teeth: An extended finite element method study. J Prosthet Dent 128, 195.e1-195.e7 (2022).
- Krell, K. V. & Rivera, E. M. A Six Year Evaluation of Cracked Teeth Diagnosed with Reversible Pulpitis: Treatment and Prognosis. J Endod 33, 1405–1407 (2007).
- Yee, K. et al. Survival Rates of Teeth with Primary Endodontic Treatment after Core/Post and Crown Placement. J Endod 44, 220–225 (2018).
- Ratcliff, S., Becker, I. M. & Quinn, L. Type and incidence of cracks in posterior teeth. Journal of Prosthetic Dentistry 86, 168–172 (2001).
- Alaugaily, I. & Azim, A. A. CBCT Patterns of Bone Loss and Clinical Predictors for the Diagnosis of Cracked Teeth and Teeth with Vertical Root Fracture. J Endod 48, 1100–1106 (2022).
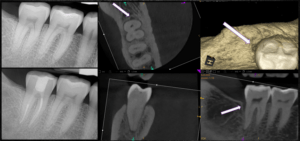
Figure 1: Pulp necrosis, acute apical periodontitis, minimally restored tooth #31 with a deep distal crack extending 5mm apical to the level of the canal orifice. Arrows highlight CAIPP on CBCT image.
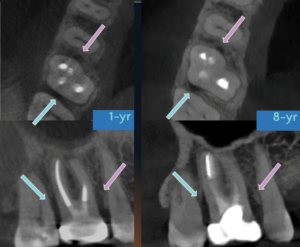
Figure 2: Very little change in CAIPP over a seven-year period. Arrows indicate CAIPPs associated with both mesial and distal deep cracks for tooth #3. At the eight-year follow-up, the patient, asymptomatic and fully functional, could not remember which tooth was treated.




