Differentiating Resorption
 By Brooke Blicher, DMD
By Brooke Blicher, DMD
The AAE Glossary of Terms defines Resorption as physiologic or pathologic loss of dentin, cementum, and/or bone not immediately due to caries or trauma. (AAE Glossary) This definition really describes what resorption is not. Truly defining resorption requires a much longer answer.
Both resorptive dental diseases and physiologic resorption associated with the exfoliation of primary teeth share a common pathogenesis. Resorption occurs when developmental precementum or predentin are lost or damaged and inflammation of the adjacent soft tissues allows for clastic cell invasion. (Tronstad) The location of this damage, and therefore the associated tissues, determines the type of resorption that occurs. Resorption cannot be simply defined as internal or external. Internal root resorption (IRR) is its own unique entity, whereas external resorption can take many forms.
IRR involves loss or damage to the predentin lining the pulp chamber or root canal spaces combined with inflammation activating odontoclasts. (Tronstad) It classically occurs following localized coronal pulp necrosis, which may occur secondary to trauma, coronal fractures, deep restorative dentistry without adequate coolant spray, or pulp capping procedures. This combined damage and localized nidus of necrotic pulp tissue incites an inflammatory reaction of the adjacent vital pulp tissue, allowing resorption to progress only until complete pulp necrosis occurs. (Wedenberg & Lindskog, Gartner et al) Scanning electron micrographs show that subclinical IRR is found quite frequently in necrotic teeth, indicating that it is likely a part of normal pathophysiology. (Gabor et al) When visible clinically or radiographically, IRR is continuous with the pulp chamber or root canal space. In the absence of a perforation, IRR is quite treatable with non-surgical root canal therapy. (Caliskan & Turkun) If IRR is perforating, the advent of bioceramic materials as well as regenerative endodontic techniques show promise. (Kaval et al)
External resorptive diseases take several forms depending on their etiology, but share the pathogenesis of loss or damage to the precementum lining the root surface combined with inflammation of the adjacent periodontal ligament, activating odontoclasts. (Tronstad) External inflammatory root resorption (EIRR) relates to endodontic pathosis. Apical EIRR is often present subclinically in cases of apical periodontitis secondary to pulp necrosis. (Vier & Figuieredo) Lateral EIRR is often more extensive, and occurs following severe luxation-type injuries or avulsions. These injuries are associated with both pulp necrosis and direct damage to the root surface, including the precementum and adjacent periodontal ligament. (Hammarstrom et al) Transient forms of lateral EIRR called “surface resorption” may occur in the early stages of healing post-trauma, but will resolve as long as pulp tissue retains vitality. (Andreasen & Kristerson) When managed in early stages, both apical and lateral EIRR often resolve with non-surgical root canal therapy.
If lateral EIRR becomes progressive, it has the potential to progress to replacement resorption, or ankylosis. Replacement resorption occurs due to bony remodeling directly follows the resorptive process. (Tronstad, Andreasen & Kristerson) Clinically, teeth lack physiologic mobility and exhibit a metallic tone on percussion. Due to continued jaw growth and passive eruption of surrounding teeth, ankylosed teeth will gradually appear to intrude. Radiographically, the periodontal ligament and lamina dura defining the root are replaced by osseous ingrowth. (Andreasen & Kristerson) No known intervention exists for replacement resorption. If enough root surface is replaced that the tooth reaches one millimeter of infraocclusion, a decoronation protocol is advised to pre-empt coronal fracture and move towards implant replacement. (Malmgren)
Pressure resorption (PR) is a non-inflammatory form of external resorption. PR is associated with the same originating tissues as EIRR via a differing etiology. It occurs secondary to direct damage to the precementum and periodontal ligament, via orthodontic movement, misaligned tooth eruption or slow-growing tumors or cysts of the jaw. (Tronstad) Removing the causative agent by stopping orthodontic movement (Zahrowski) or removing the misaligned tooth or jaw lesion will halt PR; however, resorbed tooth structures will not regrow. As pulpal disease does not cause PR, endodontic therapy is not indicated in its management. (Tronstad) Its prognosis is determined by the ability to remove the source of resorption as well as the extent of tooth loss that’s already occurred.
External cervical resorption (ECR) is the final major categorization of resorption. Empirically, ECR is the form of resorption most often seen in clinical dental practice. Technically speaking, ECR is externally derived; though, its originating tissues are distinct from the other forms of external resorption. ECR occurs at the cementoenamel junction due to developmentally missing, lost or damaged precementum, combined with inflammatory tissues in the junctional epithelium of the periodontal attachment apparatus, at the base of the gingival sulcus. (Heithersay 1999a, Patel et al 2018a) Proposed etiologies include a history of orthodontics, trauma, periodontal therapy or internal bleaching with caustic agents. However, it often presents idiopathically, and has been associated with a wide variety of other conditions, including certain viruses. (Heithersay 1999b, Patel et al 2018a) ECR can present with significant soft tissue ingrowth, wherein vascular tissue within a cervical concavity can be detected clinically, or a pink discoloration may be seen within the crown. In other cases, osseous ingrowth can occur and the lesions will be clinically undetectable. Radiographically, lesions present as mixed radiolucencies, with a ground glass appearance as the lesions extend inward. As the dental pulp has its own protective predentin, pulpal involvement is rare unless secondary caries or infection develops within the resorptive cavity. (Patel et al 2018a) Assuming the tooth is restorable, lesions are generally managed surgically, with application of trichloroacetic acid to aid debridement, followed by restoration of the defect. (Heithersay 1999c, Patel 2018b) Secondary pulpal involvement will necessitate endodontic intervention. Active monitoring can be considered in lieu of extraction for extensive and oftentimes asymptomatic lesions with osseous ingrowth reminiscent of replacement resorption.(Patel 2018b)
To avoid misdiagnosis and mismanagement of resorptive dental diseases, it behooves the clinician to be aware of these conditions. Careful attention to the location of resorbing tissue, their clinical and radiographic appearance, and the presence of any etiologic agents can make accurate detection, diagnosis and management all possible.
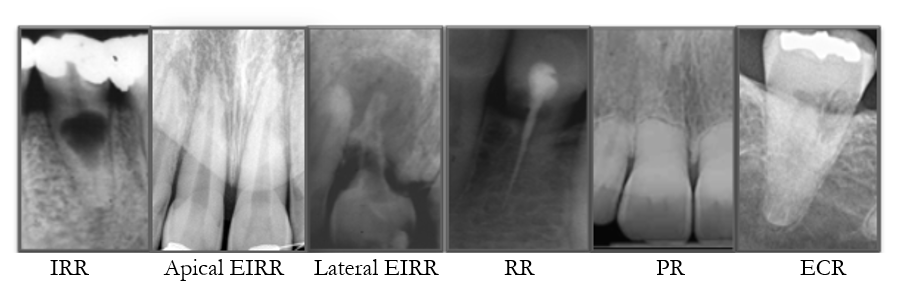
Figure 1. The varying types of resorptive dental diseases.
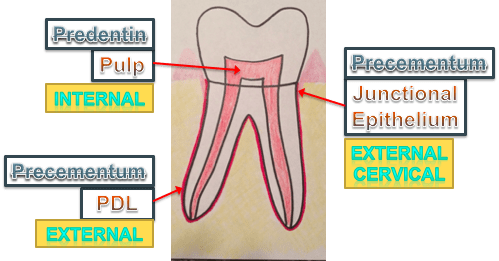
Figure 2. The pathogenesis, by tissue type, of the major types of resorption.
References
- American Association of Endodontists. Glossary of Endodontic Terms, 10th edition. www.aae.org/glossary. Accessed 22 November 2020.
- Tronstad L. Root resorption–etiology, terminology and clinical manifestations. Endod Dent Traumatol 1988;4:241-252.
- Wedenberg C, Lindskog S. Experimental internal resorption in monkey teeth. Endod Dent Traumatol 1985;1:221-7.
- Gartner AH, et al. Differential diagnosis of internal and external resorption. J Endod 1976;2:329-34.
- Gabor C, et al. Prevalence of internal inflammatory root resorption. J Endod 2012;38:24-7.
- Caliskan MK, Turkun M. Prognosis of permanent teeth with internal resorption: A clinical review. Endod Dent Traumatol 1997;13:75-81.
- Kaval ME, Güneri P, Calişkan MK. Regenerative endodontic treatment of perforated internal root resorption: A case report. Int Endod J 2018;51:128–137.
- Vier F, Figueiredo JA. Prevalence of different periapical lesions associated with human teeth and their correlation with the presence and extension of apical external root resorption. Int Endod J 2010;35:710-19.
- Andreasen JO, Kristerson L. The effect of limited drying or removal of the periodontal ligament. Periodontal healing after replantation of mature permanent incisors in monkeys. Acta Odontol Scand 1981;39:1-13.
- Hammarstrom L, et al. Tooth avulsion and replantation – A review. Endod Dent Traumatol 1986:2:1-8.
- Malmgren B. Ridge preservation/decoronation. Pediatr Dent 2013;35:164-169.
- Zahrowski J, Jeske A. Apical root resorption is associated with comprehensive orthodontic treatment but not clearly dependent on prior tooth characteristics or orthodontic techniques. J Am Dent Assoc 2011;142:66-8.
- Heithersay GS. Clinical, radiologic, and histopathologic features of invasive cervical root resorption. Quintessence Int 1999a;39:27-37.
- Patel S, Mavridou AM, Lambrechts P, Saberi N. “External cervical resorption-part 1: histopathology, distribution and presentation.” Int Endod J 2018a;51: 1205-1223.
- Heithersay GS. Invasive cervical resorption: An analysis of potential predisposing factors. Quintessence Int 1999b; 30:83-95.
- Heithersay GS. Treatment of invasive cervical resorption: An analysis of results using topical application of trichloroacetic acid, curettage, and restoration. Quintessence Int 1999c; 30:96-110
- Patel S, Foschi F, Condon R, Pimentel T, Bhuva B(2018b). “External cervical resorption: part 2 – management.” Int Endod J 2018b; 51:1224-1238.
Dr. Brooke Blicher joined Upper Valley Endodontics in 2009. She continues to teach at both Harvard and Tufts dental schools, and is on dental staff at Dartmouth-Hitchcock Medical center. An active researcher, Dr. Blicher has several publications in major dental journals.




