How Can We Provide Higher Quality Endodontic Treatment for Our Pediatric Patients?
By Su-Min Lee, DDS, MS, DScD
Pediatric patients have a greater risk of dental caries and a higher incidence of dental trauma. According to a recent systematic review and meta-analysis, the prevalence of dental caries in permanent teeth in children in the world was 53.8%. Furthermore, the frequency of dental trauma in permanent teeth of patients aged between 6 and 15 was 34.4%, with falls the most common cause of trauma. Endodontic treatment for pediatric patients is essential not only to prevent and eliminate pulpal and periapical diseases but to maintain healthy tooth development, proper form, and the function of the dentition. A previous study reported the prevalence of endodontic treatment in children is up to 9.6%. Recently, a retrospective study of pediatric patients with mixed dentition (age 6-12) was conducted to assess the prevalence and pattern of their endodontic treatment carried out at the postgraduate endodontic clinic at my institution. Pediatric patients with mixed dentition composed ~7% of all patient populations with caries as the most prevalent reason for endodontic treatment. However, a survey study among endodontists revealed that 13% of responders do not perform endodontic treatment on children. Considering that the prevalence of carious lesions and traumatic injury in a pediatric population is high, it is crucial that endodontists understand their roles and tools to treat these growing patients in need of endodontic care. However, endodontists often express extreme stress and difficulty as they treat pediatric patients who may need additional behavior management and modifications in clinical treatment.
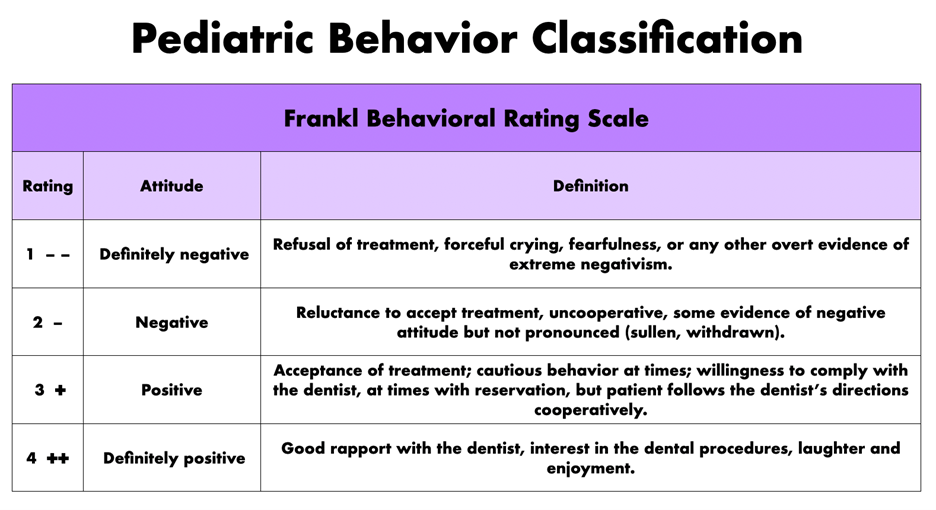
How can we improve the management of our pediatric patients? Behavior management is defined as “the process by which practitioners help patients identify appropriate and inappropriate behavior, learn problem-solving strategies and develop impulse control, empathy, and self-esteem.” The goals of behavior management are 1) to establish communication, 2) to alleviate fear and anxiety, 3) to deliver quality care, 4) to build trust, 5) to promote a positive attitude towards oral health care. Evaluation of the child’s behavior serves as an aid in directing individualized behavior guidance approach that facilitates dental treatment and provides a means for systematically recording behaviors for future appointments for pediatric dentists. Most pediatric dentists use the Frankl Behavioral Rating Scale to evaluate a child’s behavior during dental visits. The Frankl scale categorizes the child’s behavior in the dental clinic into four categories: rating 1 (definitely negative) to rating 4 (definitely positive).
There are four predictors of child behavior: patient attributes, parental influence, patient assessment, dentist/dental team behaviors, and dental environment.
1) Patient attributes: developmental delay, physical disability, or acute/chronic disease increase probability of non-compliance. Developmental age, the corresponding level of cognition, and emotionality play a prominent role in clinical behavior.
2) Parental influences: Anxiety can be transferred from parents to child, thus affecting the child’s attitude and response to care. Parents, particularly the mother, are a significant influence on the dental perception and mood of the child towards dentistry. For example, helicopter parents are parents who pay incredibly close attention to their kids’ activities and schoolwork to not only protect them from pain and disappointment but to help them succeed. Helicopter parents are known to hover over their children and become overly involved in their lives. Moreover, Lawnmower parents, the new helicopter parents, remove obstacles for their kids in hopes of setting them up to be successful. Parental presence/absence can be used to gain the patient’s cooperation. Parental involvement has changed and increased over the years. Here, the goal for a dentist is to achieve patient attention, establish dentist-child roles, and enhance effective communication, which ultimately minimizes patients’ anxiety. Parental presence/absence can be applied to any patient. However, parents unwilling or unable to extend adequate support would be a contraindication.
3) Patient assessment: evaluation of cooperative potential is essential for treatment planning. Questions about patient cognitive level behavior at medical visits should be included in medical history (e.g., How does he/she do at the pediatrician when he/she gets their vaccines? How does he/she do at the pediatric dental office for operative procedures?). A child’s temperament is broadly embraced and defined as how a child responds to novel environments and strangers. Temperament is thought to have a genetic basis, and some aspects of the temperament domain significantly influence children’s behavior in clinical settings, including dental offices. Shy or withdrawn, non-approachable, and moody children generally may not cooperate for routine dental procedures. Some data suggest that they are not good sedation candidates unless the attained depth of sedation is relatively deep.
4) Dentist/Dental Team behaviors: dentist attitude, body language, and communication skills are critical. To reduce the patient’s anxiety, clear instructions, empathetic communication, and an appropriate level of physical contact accompanied by verbal reassurance need to be used. The importance of good communication with the parent is necessary to set the stage for understanding prognostic possibilities and expectations of treatment processes their children receive, especially those who have suffered traumatic injuries. Furthermore, dentists should let children give them a STOP signal. In addition, non-clinical office staff plays an important role in behavior guidance as they are the first contact with a patient. Their tone of voice should be pleasant and welcoming.
Behavior management techniques are a set of procedures aimed at enhancing a child’s practical coping skills to achieve complete willingness and acceptance of dental care and ultimately reduce the child’s perception that the dental situation is overwhelming or dangerous. The non-pharmacological behavior management technique decreases fear and avoidance and increases patients’ self-efficacy to get patients through the procedure without pharmacological risk. However, it often requires a long time to achieve good patient cooperation by dental standards. If traditional techniques become unsuccessful in managing behavior, pharmacological behavior management, sedation needs to be considered. Phobic, excessively fearful children, and older children with poor experiences or coping abilities are generally an indication for sedation. Patients in ASA classes I and II are frequently considered appropriate candidates for minimal, moderate, or deep sedation. Children in ASA classes III and IV, children with special needs, and those with anatomic airway abnormalities or moderate to severe tonsillar hypertrophy require additional individual consideration, particularly for moderate and deep sedation.
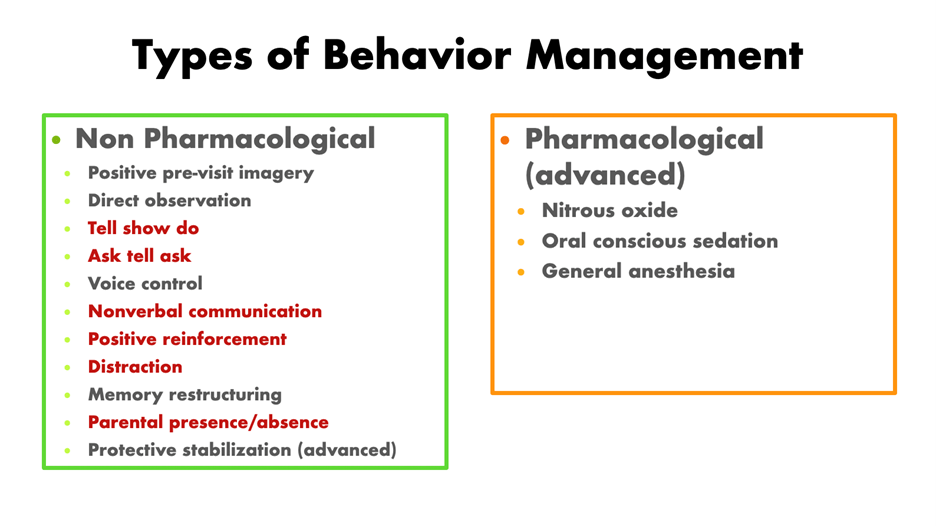
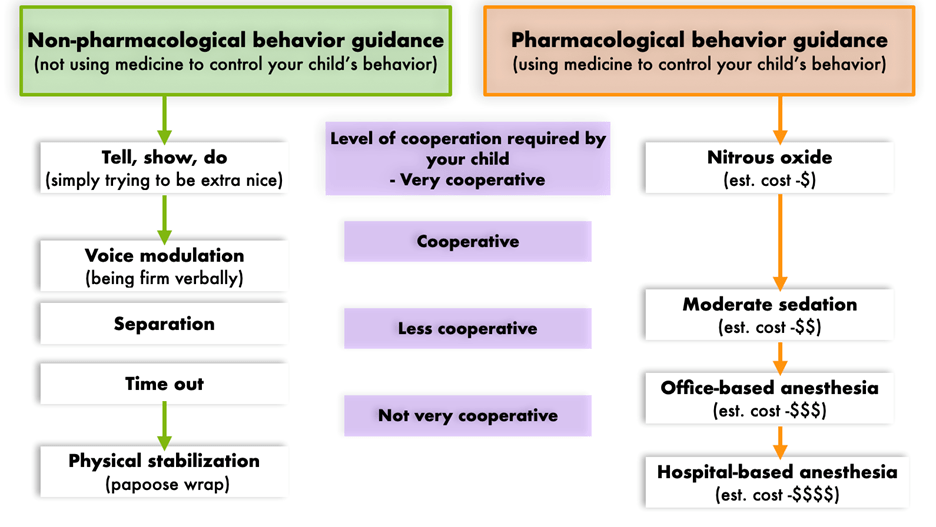
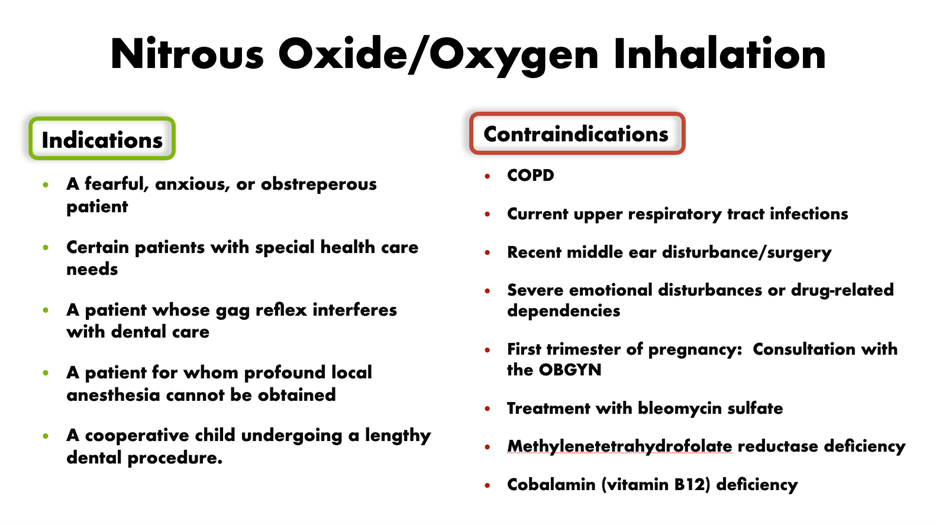
Nitrous oxide/oxygen (N₂O/O₂) inhalation sedation is a commonly used form of pharmacological behavior management for pediatric patients. According to a study about the parental attitude toward behavior management techniques, nitrous oxide sedation was the second greatest acceptance following “tell-show-do” among eight proposed behavior management techniques. A recent retrospective study showed that 94% of behavior-challenging children successfully received root canal treatment on permanent teeth under N₂O (50%)/O₂ (50%) sedation with midazolam in combination with meperidine or hydroxyzine. For the endodontic procedure, nitrous oxide should be considered as the first choice for sedative management. Endodontists need to receive training for behavioral management and sedation techniques in order to perform planned endodontic procedures and achieve optimal patient care results.
Reference
Mohsen Kazeminia, Alireza Abdi, Shamarina Shohaimi, Rostam Jalali, Aliakbar Vaisi-Raygani, Nader Salari, Masoud Mohammadi. Dental caries in primary and permanent teeth in children’s worldwide, 1995 to 2019: a systematic review and meta-analysis. Head Face Med 2020 Oct 6;16(1):22.
Thais Rodrigues Campos Soares, Patricia de Andrade Risso, Lucianne Cople Maia. Traumatic dental injury in permanent teeth of young patients attended at the federal University of Rio de Janeiro, Brazil. Dental Traumatol 2014 Aug;30(4):312-6.
Ridell Karin, Matsson Lars, Mejàre Ingegerd. Background factors associated with endodontic treatment due to caries in young permanent teeth. Acta Odontol Scand 2007;65(4):219–23.
Popoola B O, Ayebameru O E, Olanloye O M. Endodontic Treatment in Children: A Five-Year Retrospective Study of Cases Seen at the University College Hospital, Ibadan, Nigeria. Ann Ibadan Postgrad Med 2018;16(2):136–41.
AAE21 Abstracts of Research. https://doi.org/10.1016/S0099-2399(21)00373-3
St Paul Alison, Phillips Ceib, Lee Jessica Y., Khan Asma A. Provider Perceptions of Treatment Options for Immature Permanent Teeth. J Endod 2017;43(6):910–5.
Wilson Stephen. Management of Child Patient Behavior: Quality of Care, Fear and Anxiety, and the Child Patient. J Endod 2013;39(3):S73–7.
Townsend Janice A., Wells Martha H. Behavior Guidance of the Pediatric Dental Patient. Pediatr. Dent. Elsevier; 2019. p. 352-370.e2.
Coté Charles J., Wilson Stephen. Guidelines for Monitoring and Management of Pediatric Patients Before, During, and After Sedation for Diagnostic and Therapeutic Procedures. Pediatrics 2019;143(6):e20191000.
Eaton Jonathan J., McTigue Dennis J., Fields Henry W., Beck Michael. Attitudes of contemporary parents toward behavior management techniques used in pediatric dentistry. Pediatr Dent 2005;27(2):107–13.
American Academy on Pediatric Dentistry Council on Clinical Affairs. Policy on the use of deep sedation and general anesthesia in the pediatric dental office. Pediatr Dent 2008;30(7 Suppl):66–7.




