Vital Pulp Therapy for Children
By Xu Han, DDS MS
Thirteen-year-old Jane (name has been changed for HIPAA) was an established patient at a local community clinic. She missed a few recall visits during the pandemic years but returned with pain in her lower right. A temporary restoration was placed at the community clinic. Due to high anxiety and lack of cooperation, neither the community clinic nor the endodontist she was referred to were able to provide the definitive pulp treatment that she needed.
As a last resort, Jane ended up in the chair of a third-year dental student. The dental student successfully managed her anxiety, selectively removed caries and performed indirect pulp therapy using Biodentine. The tooth has been asymptomatic for six months (as of August 2024) with normal apical tissue. Pulp testing is needed to confirm vitality at the next recall visit in the student clinic.

Vital pulp therapy (VPT) for permanent teeth in children presents unique challenges to the general and specialty dental provider.
Working with children is difficult.
Children are resilient, whether they are nine or thirteen years old. The circumstance that led Jane to the chair of a third-year dental student is evidence of that. Managing behavior and understanding pediatric growth allowed an inexperienced dental student to be successful.
Behavior management can be broken down into two categories: people and technique. Every person in the treatment room can affect the clinical outcome. What if thirteen-year-old Jane started out calm? If we had a helicopter dad and a nervous dental student, Jane may have developed anxiety during the appointment. Technique is just as important. Delaying treatment by a few hours may allow an upset child to calm down emotionally. Success of pediatric local anesthesia is not just measured by the absence of pain during treatment, but during its administration. While rubber dam isolation is the gold standard, we can’t abandon treatment for all children that physically can’t tolerate its use.
Understanding the development of a child’s tooth is as important as understanding their overall growth. A tooth with an open apex has greater vascular supply, which boosts its ability to heal. The stage of root development impact sensibility testing; and poor enamel quality like hypo-mineralization impacts restorability and the ability to achieve profound anesthesia. On a growth level, a child may present with a narrow palate and restricted tissue plasticity. This child may not physically be able to tolerate radiographs and subsequent treatment. Finally, it’s important to evaluate dental age and arch space discrepancy as we consider molar substitution.
Future Opportunities
Consider the following panoramic radiograph of a 9.5-year-old patient from my practice. How would you treat this patient as an endodontist? What would a general dentist or pediatric dentist do?
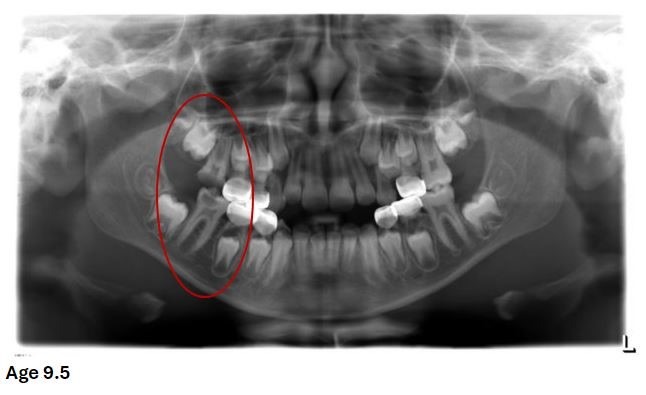
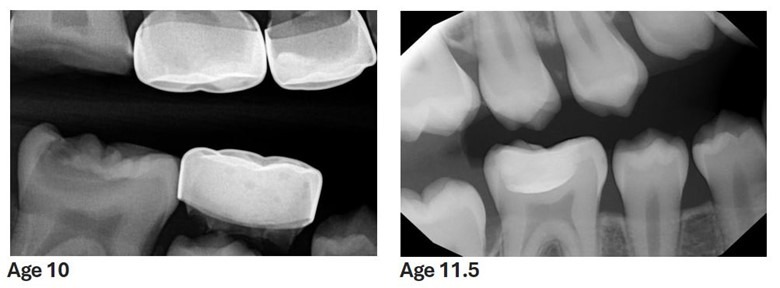
The patient did not immediately return for the recommended treatment. At age 10, I took her to a local children’s hospital, where I extracted #3 and restored #30 with an indirect pulp cap (calcium silicate cement and composite) while the patient was under general anesthesia. Timely molar substitution allowed #2 to erupt into the vacated space of #3 by age 11.5.
Dr. Xu Han is Diplomate, American Board of Pediatric Dentistry and Clinical Director, TDS Pediatric Dentistry.




