Beyond the Radiograph: Histological Insights into Human Mature and Immature Teeth in Regenerative Endodontics
By Badr Hefnawi, Raju Gandhi, and Xiaofei Zhu
Many clinicians have ventured into the realm of regenerative procedures, often presenting radiographic evidence of apical closure and canal wall thickening. These observations frequently lead to assertions of successful regeneration. However, it is vital to acknowledge that relying solely on radiographic assessments cannot definitively distinguish between repair and regeneration (Figure 1). A deeper dive must be taken into the histological outcomes of regenerative procedures to attain a better understanding of its success.
Many prospective animal studies have been conducted to examine the histological outcomes to various treatment methods, however results from animal studies may not always be extrapolated to human situations.1,2,3 This is due to variations in pathophysiology, and also different study protocol conditions that can take place in animal versus human studies. Due to ethical reasons, no randomized control trial has been conducted in humans on histological outcomes. This limits the current review to focus on human histological observational studies as opposed to interventional. Although the number of reports on in vivo teeth that have undergone REP followed by histological analysis is scarce, and the details of each treatment may vary, it does not take away from the importance of evaluating this body of literature.
Literature Search
A comprehensive literature search was conducted across PubMed, Embase, and Web of Science for studies published between 2001 and 2023. Inclusion criteria required that each study report a completed regenerative endodontic procedure with histological evaluation—either of the entire tooth or a relevant section. Out of 389 initially identified papers, 17 human case studies were ultimately included, representing 22 teeth subjected to histological analysis.
Pre-Treatment Diagnoses and Patient Demographics
Of the 22 teeth reviewed, 18 were immature teeth, most diagnosed with pulp necrosis and apical pathology such as acute or chronic apical abscesses, symptomatic or asymptomatic apical periodontitis. These align with the classic indications for REP, where continued root development is desired.4-20
Two cases involved mature teeth with pulpal necrosis—an area of increasing interest in regenerative endodontics. Notably, two additional cases featured vital, healthy teeth undergoing REP strictly for research purposes before scheduled orthodontic extraction, providing rare control-like conditions.
Clinical Outcomes
Thermal or electric pulp testing was included as part of the evaluations in 19 of the 22 cases reviewed. Five of these teeth recorded a positive reaction to either thermal or electric pulp testing. Notably, two of these teeth cases were mature teeth that belonged to the only case report involving mature teeth with histologic examination. These teeth lasted 3.5 years before requiring extraction due to horizontal crown fractures. These cases demonstrate the potential of regenerative procedures to induce a positive sensibility response in mature teeth, even in necrotic cases.
Percussion testing was reported in 20 of the 22 cases reviewed, with five teeth showing a positive response. Three of these teeth also showed a response to either thermal or electric pulp testing. The remaining two teeth that tested positive to percussion were associated with persistent infection, demonstrated by an acute apical abscess in one case and symptomatic apical periodontitis in the other.
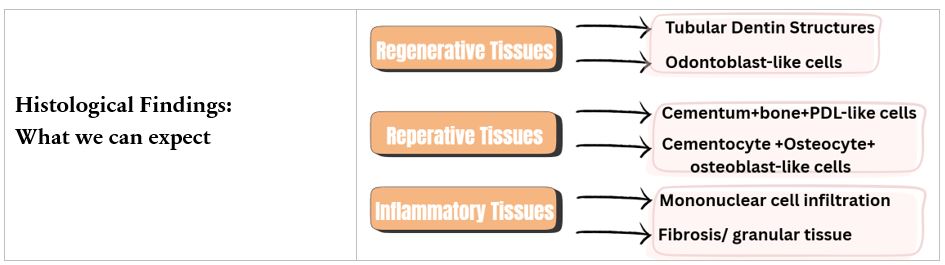
Figure 1: Histological spectrum of outcomes following regenerative endodontic procedures. Regenerative response showing formation of tubular dentin structures and odontoblast-like cells, indicative of true pulp–dentin complex regeneration. Reparative response characterized by cementum-, bone-, and periodontal ligament (PDL)-like tissues containing cementocyte, osteocyte, and osteoblast-like cells. Inflammatory response demonstrating mononuclear cell infiltration with fibrotic or granular tissue formation, reflecting an unfavorable healing outcome.
Histological findings
The distribution of tissue responses following regenerative procedures varied according to the underlying etiology (Figure 2). Reparative outcomes were the most frequently observed across all categories, with caries and crown fractures demonstrating the highest number of cases. Dens evaginatus, however, showed a broader spectrum of outcomes, including combined reparative–regenerative and reparative–inflammatory responses, highlighting the complexity of tissue reactions in this condition. In contrast, purely regenerative or inflammatory responses were relatively uncommon overall.
While these findings may, in part, reflect the bacterial nature of certain etiologies, definitive conclusions cannot be drawn due to variability in protocols, including differences in materials, intracanal medicaments, and treatment time frames.
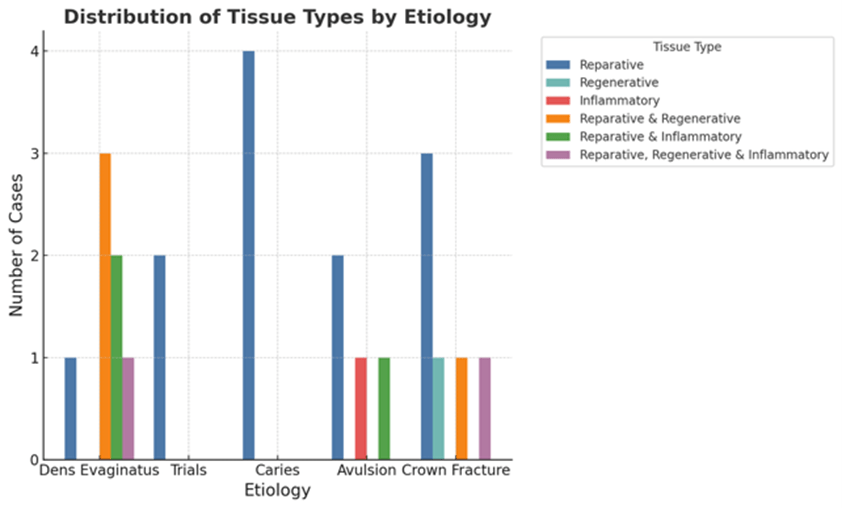
Figure 2: Distribution of regenerative, reparative, and inflammatory histological findings across human teeth subjected to regenerative procedures, categorized by etiology.
Comparing Immature and Mature Teeth
Although most studies involved immature teeth, the mature tooth cases may be the most groundbreaking.4,5 Histological analysis of these teeth (combined with clinical testing) demonstrates true regeneration may be possible even without a natural apical blood supply or native stem cells. This could represent a shift in the field’s understanding and a call to expand REP indications, particularly as tissue engineering advances, including the use of platelet-rich/fibrin matrices and allogenic stem cells, continue to emerge.
Conclusion: Regeneration or Repair?
This review provides a nuanced look into the biological realities of regenerative endodontic procedures in humans. While true pulp regeneration remains elusive, the formation of vascularized, functional tissue in some cases, especially in mature teeth, marks an encouraging evolution in endodontic care. As protocols are refined and regenerative materials evolve, a future where true pulp regeneration is routine may not be far off. Until then, continuing to integrate histological insights into clinical decision-making will be key in ensuring REP fulfills its promise.
References
- Altaii M, Richards L, Rossi-Fedele G. 2017. Histological assessment of regenerative endodontic treatment in animal studies with different scaffolds: A systematic review. Dent Traumatol. 33(4):235-244.
- Torabinejad M, Faras H, Corr R, Wright KR, Shabahang S. 2014. Histologic examinations of teeth treated with 2 scaffolds: A pilot animal investigation. J Endod. 40(4):515-520.
- Yamauchi N, Yamauchi S, Nagaoka H, Duggan D, Zhong S, Lee SM, Teixeira FB, Yamauchi M. 2011. Tissue engineering strategies for immature teeth with apical periodontitis. J Endod. 37(3):390-397.
- Adhikari HD, Gupta A. 2018. Report of a case of platelet-rich fibrin-mediated revascularization of immature 12 with histopathological evaluation. J Conserv Dent. 21(6):691-695.
- Arslan H, Şahin Y, Topçuoğlu HS, Gündoğdu B. 2019. Histologic evaluation of regenerated tissues in the pulp spaces of teeth with mature roots at the time of the regenerative endodontic procedures. J Endod. 45(11):1384-1389.
- Austah O, Joon R, Fath WM, Chrepa V, Diogenes A, Ezeldeen M, Couve E, Ruparel NB. 2018. Comprehensive characterization of 2 immature teeth treated with regenerative endodontic procedures. J Endod. 44(12):1802-1811.
- Becerra P, Ricucci D, Loghin S, Gibbs JL, Lin LM. 2014. Histologic study of a human immature permanent premolar with chronic apical abscess after revascularization/revitalization. J Endod. 40(1):133-139.
- Kwon SK, Kyeong M, Adasooriya D, Cho SW, Jung IY. 2023. Histologic and electron microscopic characterization of a human immature permanent premolar with chronic apical abscess 16 years after regenerative endodontic procedures. J Endod. 49(8):1051-1057.
- Lei L, Chen Y, Zhou R, Huang X, Cai Z. 2015. Histologic and immunohistochemical findings of a human immature permanent tooth with apical periodontitis after regenerative endodontic treatment. J Endod. 41(7):1172-1179.
- Lin LM, Shimizu E, Gibbs JL, Loghin S, Ricucci D. 2014. Histologic and histobacteriologic observations of failed revascularization/revitalization therapy: A case report. J Endod. 40(2):291-295.
- Lui JN, Lim WY, Ricucci D. 2020. An immunofluorescence study to analyze wound healing outcomes of regenerative endodontics in an immature premolar with chronic apical abscess. J Endod. 46(5):627-640.
- Martin G, Ricucci D, Gibbs JL, Lin LM. 2013. Histological findings of revascularized/revitalized immature permanent molar with apical periodontitis using platelet-rich plasma. J Endod. 39(1):138-144.
- Meschi N, Hilkens P, Van Gorp G, Strijbos O, Mavridou A, Cadenas de Llano Perula M, Lambrichts I, Verbeken E, Lambrechts P. 2019. Regenerative endodontic procedures posttrauma: Immunohistologic analysis of a retrospective series of failed cases. J Endod. 45(4):427-434.
- Nosrat A, Kolahdouzan A, Hosseini F, Mehrizi EA, Verma P, Torabinejad M. 2015. Histologic outcomes of uninfected human immature teeth treated with regenerative endodontics: 2 case reports. J Endod. 41(10):1725-1729.
- Palma PJ, Martins J, Diogo P, Sequeira D, Ramos JC, Diogenes A, Santos JM. 2019. Does apical papilla survive and develop in apical periodontitis presence after regenerative endodontic procedures? Appl Sci. 9(19):3942.
- Peng C, Zhao Y, Wang W, Yang Y, Qin M, Ge L. 2017. Histologic findings of a human immature revascularized/regenerated tooth with symptomatic irreversible pulpitis. J Endod. 43(6):905-909.
- Shetty H, Shetty S, Kakade A, Desai R, Zhang CF, Neelakantan P. 2018. Cone-beam computed tomographic and histological investigation of regenerative endodontic procedure in an immature mandibular second premolar with chronic apical abscess. J Investig Clin Dent. 9(4):e12352.
- Shimizu E, Jong G, Partridge N, Rosenberg PA, Lin LM. 2012. Histologic observation of a human immature permanent tooth with irreversible pulpitis after revascularization/regeneration procedure. J Endod. 38(9):1293-1297.
- Shimizu E, Ricucci D, Albert J, Alobaid AS, Gibbs JL, Huang GT, Lin LM. 2013. Clinical, radiographic, and histological observation of a human immature permanent tooth with chronic apical abscess after revitalization treatment. J Endod. 39(8):1078-1083.
- Torabinejad M, Turman M. 2011. Revitalization of tooth with necrotic pulp and open apex by using platelet-rich plasma: A case report. J Endod. 37(2):265-268.
Badr Hefnawi, Raju Gandhi, and Xiaofei Zhu are with the Department of Endodontics, Boston University Henry M. Goldman School of Dental Medicine.
