Antibiotics: A Risky Prescription
By Richard E. Walton, D.M.D., M.S.
 The adverse effects of overusing and misusing antibiotics are highly publicized in the health professional literature, most recently in the August issue of the Journal of the American Dental Association.1 According to the Centers for Disease Control and Prevention, more than 2 million people in the United States are hospitalized and more than 23,000 die each year from superinfections caused by antibiotic-resistant bacteria.2Clostridium difficile is a particularly vicious resistant bacterium. A major two-year review of antimicrobial resistance reached the grim conclusion that, without drastic curbs, drug-resistant superbugs could claim millions of lives worldwide each year. These superbugs have the potential to become a greater killer than cancer by 2050.3 Yet, despite the potential dangers and limited usefulness of antibiotics in dentistry and endodontics, their use is common and possibly increasing.4
The adverse effects of overusing and misusing antibiotics are highly publicized in the health professional literature, most recently in the August issue of the Journal of the American Dental Association.1 According to the Centers for Disease Control and Prevention, more than 2 million people in the United States are hospitalized and more than 23,000 die each year from superinfections caused by antibiotic-resistant bacteria.2Clostridium difficile is a particularly vicious resistant bacterium. A major two-year review of antimicrobial resistance reached the grim conclusion that, without drastic curbs, drug-resistant superbugs could claim millions of lives worldwide each year. These superbugs have the potential to become a greater killer than cancer by 2050.3 Yet, despite the potential dangers and limited usefulness of antibiotics in dentistry and endodontics, their use is common and possibly increasing.4
Why are antibiotics prescribed so frequently?
Although antibiotics are prescribed for a variety of dental concerns, they are often sought out for real or perceived endodontic problems.5, 6, 7 Why is this? While there are no data on the reasons, I suspect that the following factors come into play:
- Antibiotics seem to "work." If a patient with a real or perceived endodontic problem is prescribed an antibiotic, with or without corresponding treatment, they often improve. The antibiotics are considered to be the major contributor, but the placebo effect likely plays a role. Pain cycles up and down spontaneously, and pain from an endodontic emergency has been shown to decrease, even without treatment of the tooth.8 Controlled trials show that antibiotics are unrelated to the resolution of signs and symptoms and that antibiotics are ineffective in managing pain.9
- Old habits die hard. If antibiotics have been incorporated into the practice, there is built-in reluctance to change.
- Endodontists want to help their patients. We want to come to our patients' aid when they are in distress, but prescribing antibiotics is not the answer. In fact, there is convincing evidence that antibiotics are ineffective for localized pathosis.10
- Patients expect antibiotics. There is a belief that antibiotics are "miracle drugs" that will resolve most adverse problems. Patients also are putting their trust in the judgment of their healthcare providers.
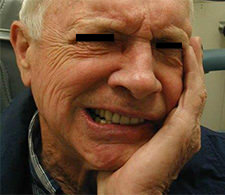
- Antibiotics are believed to prevent the spread of infection. This belief often is a factor in cases of acute apical abscesses, although the evidence shows that antibiotics are not preventative.11, 12Debridement and drainage usually resolve the problem fairly quickly, as was the case with a patient who presented with a localized apical abscess that developed as a result of pulp necrosis from the incisor (Figure 1). The only exception is cellulitis, for which penicillin is recommended.
- Antibiotics are believed to minimize adverse post-endodontic events. This is another commonly held belief; yet, clinical trials show that antibiotics are unrelated to post-treatment signs and symptoms.13, 14
- No one wants a lawsuit. Litigation is a valid concern; the dentist is understandably anxious to avoid being sued for substandard treatment. However, if a patient attempts to sue after experiencing a problem (and antibiotics were not prescribed), the dentist is on defensible grounds. On the contrary, if antibiotics result in mortality or morbidity, this is an indefensible position. Both the dangers and lack of effectiveness are conclusive. Indeed, there have been lawsuits against dentists on this basis.
 |
 |
|
| Figure 1. A localized apical abscess(left) developed as related to pulp necrosis from the incisor(right). Debridement and drainage resulted in rapid resolution. Antibiotics were not indicated. Images courtesy of Dr. Richard Walton. | ||
What does the evidence say?
Clinical trials13, 14 and a systematic review10 have shown conclusively that antibiotics neither control nor prevent11, 12 localized endodontic pathosis, including symptomatic irreversible pulpitis.15 In one case of a patient experiencing severe pain related to symptomatic irreversible pulpitis, a partial pulpectomy effectively resolved the symptoms (Figure 2). In addition, while antibiotics have been mentioned as an adjunct or primary therapy with a number of procedures related to endodontics, including surgery, the data show that antibiotics have no impact on postsurgical outcomes.16 Another frequently mentioned recommendation for antibiotics is for so-called "systemic signs" such as elevated temperature, malaise and lymphadenopathy. Campanelli et al. found these to not occur with apical abscess.17
 |
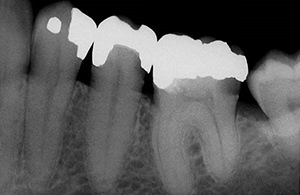 |
| Figure 2. Severe, spontaneous pain(left) related to symptomatic irreversible pulpitis as associated with this molar(right). Partial pulpectomy effectively resolved the symptoms; antibiotics were contraindicated. Images courtesy of Dr. Richard Walton. | |
When is the use of antibiotics appropriate?
In 2012, Dr. Steven G. Morrow authored an issue of the AAE's ENDODONTICS: Colleagues for Excellence newsletter on the "Use and Abuse of Antibiotics." In the issue, Dr. Morrow examines several myths regarding when antibiotics are indicated and contraindicated. A prior issue of Colleagues, "Antibiotics and the Treatment of Endodontics Infections," authored by Dr. J. Craig Baumgartner in 2006, provides recommendations for the responsible use of antibiotics in endodontic treatment. For example, cellulitis is an endodontic infection that does carry a recommendation for penicillin. Cellulitis is an infrequent, rapidly progressing, distorting swelling that often includes fascial spaces, and is potentially serious (Figures 3 and 4). Though there are no clinical trials (and likely never will be) to determine whether antibiotics are of assistance with a cellulitis, a pharmaco-therapeutic rationale for their use does exist.18
 |
| Figure 3. An 11-year-old patient developed pulp necrosis and apical pathosis from luxation injury to a canine. Severe, distorting swelling developed over a period of hours. This is cellulitis, which is infrequent but may be dramatic and is potentially dangerous. Treatment was canal debridement, intraoral incision for drainage and adjunctive potassium penicillin. Image courtesy of Dr. Richard Walton. |
 |
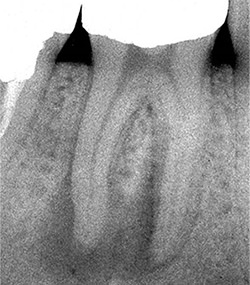 |
| Figure 4. Serious cellulitis has involved the submandibular and submylohyoid spaces (left). The origin is the necrotic pulp (right). The patient was hospitalized. The tooth was extracted and extraoral drainage performed by an oral surgeon. Potassium penicillin was administered intravenously. Images courtesy of Dr. Richard Walton. | |
What can endodontists do?
As endodontists, we have a responsibility to become part of the solution to the antibiotic resistance crisis. We do this by:
- Being responsible in our use of antibiotics. They should be prescribed only in special cases, such as cellulitis and certain medical conditions as a prophylaxis.
- Educating our patients. We can explain that antibiotics have been shown to be ineffective and may have serious side effects. They should be saved for the medical conditions for which they have shown to be useful.
- Educating our referring dentists. The overprescribing of antibiotics is a large problem that requires a group effort. General dentists are part of the solution as well.
Antibiotics have limited benefits in dentistry, and their overuse and misuse pose significant risks to our patients. As endodontists, we can do our part to minimize the spread of antibiotic-resistant bacteria by educating ourselves, our patients and our referring dentists about these risks and being judicious in prescribing antibiotics.
Dr. Richard E. Walton is professor emeritus of endodontics at the University of Iowa College of Dentistry, where he also served as endodontics department chair for 14 years. He has published extensively in clinical and basic literature and is a past recipient of the AAE's Louis I. Grossman and I.B. Bender Lifetime Educator Awards. He can be reached at richard-walton@uiowa.edu.
References:
2. Review on Antimicrobial Resistance. Antimicrobial resistance: tackling a crisis for the health and wealth of nations, 2014. Accessed July 16, 2016.
3. Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States, 2013. Accessed July 16, 2016.




