Is Retreatment Always Necessary Before Endodontic Surgery?
 By Adham A. Azim BDS, DDS
By Adham A. Azim BDS, DDS
”Retreatment first before surgery!” A statement that is still preached during endodontic training and carried from one endodontic generation to the other. The justification for this approach has been derived from classical papers suggesting improved outcomes when non-surgical retreatment (RET) is combined with endodontic surgery, compared to surgery alone (1). While historically, endodontic surgery, or to be more specific, “Traditional Surgery” had a poor outcome of around 60% (2) and RET may provide additional benefits, In today’s practice, we no longer perform traditional surgery but rather “Endodontic Microsurgery” (EMS). EMS has consistently shown high success and survival rates that are similar and even surpass RET in some studies (2-6). Despite the overwhelming evidence in the last decade regarding the predictability of EMS, RET is often proposed as the first-line of treatment for a failed root canal treatment (RCT), and surgical options are considered only if RET was not effective in the treatment of apical periodontitis (7).
To correctly answer the question above, perhaps it’s essential to challenge our treatment philosophies with several other questions:
Question 1: Why do non-surgical and surgical endodontic treatment fail?
We can narrow down the causes of RCT failure into five main causes:
- Intra-radicular biofilm
Endodontists are well aware of the complexity of root canal morphology. While we do our best to address the various atomical spaces using our instruments, irrigants, and medicaments, there is an inherent limitation of RCT to sterilize and seal all portals of entry and exit. It has been shown to be present in 77% of failed endodontic cases(8). - Extra-radicular biofilm
It has been shown that intra-radicular biofilms could extend on the outer root surface, forming an extra-radicular biofilm “like a plaque”. Even if, hypothetically, we were able to sterilize the canal, we will still not clean the outer root surface. Thankfully the incidence of extra-radicular biofilm is low, ranging between 4-6% (8, 9). However, most recently, Ricucci et al. (10) showed that this incident could increase to 77% in cases with sinus tracts, which may explain the lower success rate of these cases when managed non-surgically (11). Apical actinomycosis is another rare form of extra-radicular infection that occurs in around 1-2% of cases subjected to apical surgery, where bacteria can survive within the periapical lesions and thus won’t be addressed with any non-surgical approach (12). - True cystic lesions
While the primary cause for a true periapical cystic lesion to be present is an intra-radicular infection, it is believed that a true cystic lesion would not resolve without surgical intervention, despite adequate disinfection of the root canal system (13). True cysts have been shown to occur in around 9% of cases subjected to apical surgery (14). - Procedural errors
Having broken instruments or transportations that alters the root canal morphology would result in difficulty to adequality clean and seal the canals, and untimely a lower success rate (15). - Vertical root fractures (VRF) occurring in around 4% of cases subjected to RCT (16).
On the other hand, the causes of failure in EMS today are only limited to:
- Procedural errors performed during the surgery in the form of a missed canal, root perforation during retro-preparation, or inadequate seal of the apical area (17).
- VRF, which is also around 4%, similar to non-surgical treatment (16).
Causes 1-4 of failure following RCT can only be addressed by surgical intervention. That can explain why most recently EMS have shown superior outcome to RET among the same group of clinicians (5).
Question 2: What’s wrong with retreatment first?
In addition to the increased cost and time of treatment, RET can potentially reduce the success rate of EMS by inducing dentinal defects at the apical area (18). These defects can expand and propagate during ultrasonic retro-preparation to cracks (19) and result in a lower success rate of EMS (20). It has been recently shown by von Arx et al. (16) that RET before surgery was a risk factor for the development of VRFs following EMS.
Question 3: Would EMS be successful if attempted on a case with a poor RCT?
The quality of the root canal before the surgery has often been presented as a potential predictor for surgical failure (21). However, that is primarily derived from the way we perform EMS. We have been trained that EMS is performed by cutting the apical 3mm of the root, retro-preparation using ultrasonics, and placement of a retro-filling material. While this approach is very predictable when the quality of RCT is adequate or if we attempted RET first, it will not be as predictable when the quality of the root canal is poor (21). What often complicates the decision-making process is the presence of a large post or a long-span bridge, making RET a high-risk procedure that can compromise the tooth and/or the restoration.
For these cases, complete retreatment of the root from the surgical end should be performed by attempting a longer retro-preparation. This approach was proposed by Friedman more than 30 years ago by the use of hand files (1). While it can be technically difficult and time-consuming to hand file the canal from the apical end, today, we have ultrasonic tips that allow up to 9mm retro-preparations in a predictable, fast and safe manner. It will allow complete retreatment of the root from the surgical end while preserving the integrating of the restoration and reducing the cost and time of the treatment. It has been shown by Azim and colleagues that the quality of the RCT did not affect the outcome of EMS when longer retro-preparations were performed on cases with poor RCT quality (17). (Figure 1)
Question 4: When to consider retreatment before surgery?
There are three scenarios where RET would be advantageous before attempting EMS.
1. Cases with poor RCT and complex morphology (mandibular or maxillary molars)
These cases are likely not good candidates for longer retro-preparations due to the limited accessibility and the curvatures associated with these roots. Attempting longer retro-preparations is likely to cause procedural errors. Also, performing only a 3mm preparation is likely to have a poor prognosis (21). Thus, RET followed by EMS will result in a more predictable outcome (Figure 2).
2. Surgically inaccessible roots with a simple root canal system
Inaccessible roots such as the palatal roots of maxillary molars often have a single large canal. If it requires apical surgery, the visibility and accessibility for retro-preparation and retro-filling are often compromised. Selective retreatment can be performed on just the palatal root through a small access cavity, and the root can be filled with a root repair material. During the surgery, the root can be just resected without the need for retro-preparation or retro-filling (22) (Figure 3). This approach may only apply to inaccessible roots with a simple root canal system (No isthmus).
3. Poor RCT in simple root canal systems without coronal obstructions (No posts)
While EMS may appear as a suitable treatment approach when addressing large periapical pathologies or re-surgery cases. Performing longer retro-preparations on cases with poor RCT can be time-consuming and may cause procedural errors (Figure 4A-D). Clinicians can consider RET of the root prior to the surgery. However, there is no need to obturate the root. The canal can be left empty and filled entirely from the surgical end using a combination of BC sealer and BC putty root repair material (Figure 4E-H). This approach can have several advantages:
a. Eliminate the risk of defects propagation induced by ultrasonic tips during EMS (19)
b. Achieving the best of both worlds, ultimate disinfection through RET and ultimate apical seal during EMS.
c. Completing the treatment is a single visit by doing half RET (no obturation) and half EMS (no retro-preparation).
Another approach can also include ortho-grade filling of the root with a root repair material like we mentioned earlier, and the surgery can be limited to only apical resection (Figure 4I-L). This approach can be more suitable if the root apex is wide/open and short. In cases with long roots and narrow canals, the treatment can be significantly faster and less complex if the root is filled from the surgical end.
The 5th and last question would be, “Is endodontic surgery a treatment option or a treatment sequence?”.
Endodontic surgery has been historically practiced as a treatment sequence. “Retreat first!” If surgery is exercised as an independent treatment option, it can provide a great advantage to our patients. It can improve the outcome and reduce the time and cost of several failed primary RCTs. Therefore, I consider the following in the decision-making process for failed RCTs (Figure 5). Clinicians should first assess the quality of the coronal restoration followed by the quality of the root canal. If the restoration is poor, RET is likely to be more appropriate. If the restoration is adequate, the quality of the RCT should then be evaluated. If the RCT quality appears adequate, surgery is likely to be more appropriate. If the RCT quality is poor, then the decision to proceed with a surgical or a non-surgical approach should be based on the level of complexity (LOC) of the case, if treated surgically vs. non-surgically. Criteria similar to the American Board of Endodontics (ABE) can be used as a guide for this purpose. If a case has a higher LOC if managed non-surgically compared to a lower LOC if managed surgically, then surgery would be the treatment plan of choice, and vice versa. If the outcome is the same, it is wiser to choose a treatment plan with the lowest LOC, as the prognosis is likely to be more favorable when the procedure is less complex.
Figures:
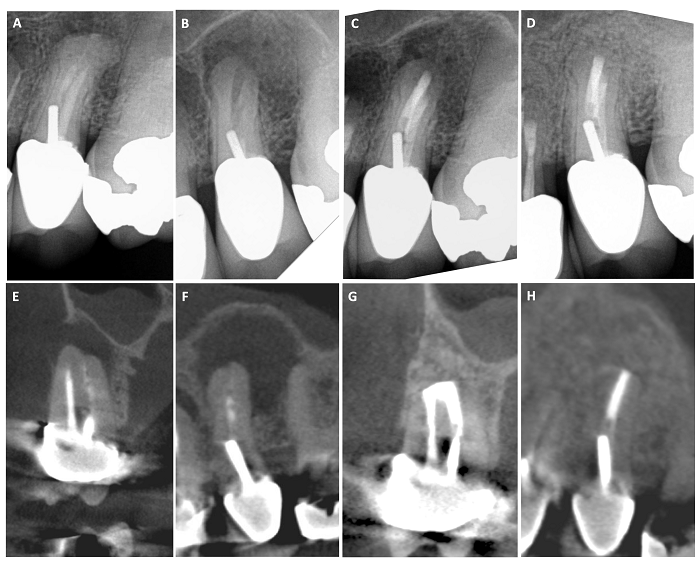
Figure 1: Management of a maxillary premolar with a poor root canal quality using long retro-preparation
(A) Pre-operative radiograph (B) intra-operative radiograph after complete removal of the root canal filling material using long retro-preparations (C) Post-operative radiograph after placement of retro-filling material (BC sealer + BC putty). (D) 1 yr. follow up showing complete apical healing. (E & F) pre-operative scan images showing large apical area and a faint root canal filling in the buccal and palatal canals (G & H): 1 yr. follow up scan images showing complete bone formation at the surgical site with retro-filling material sealing the entire buccal and palatal canals to the post level and a 3mm retro-filling in the isthmus communication.
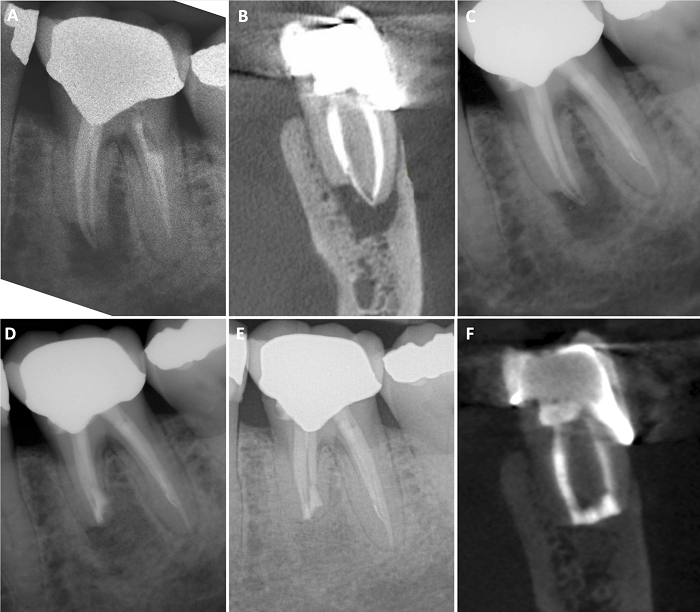
Figure 2: Management of a mandibular molar with poor RCT and apical root resorption, that required RET prior to EMS.
(A) Pre-operative radiograph (B) Pre-operative scan images showing apical resorption of the mesial root. (C) After RET (D) After EMS on the mesial root (E-F) 1 yr. follow up PA & scan showing complete healing.
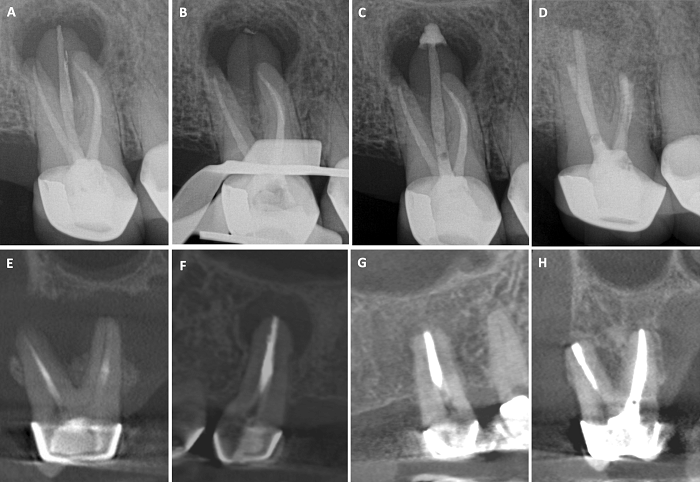
Figure 3: Management of a maxillary 2nd molar not responding to Non-surgical endodontic treatment using selective RET and EMS (in conjunction with Dr. Maksim Serebro).
(A) Pre-operative radiograph (B) selective RET of the palatal root (C) Obturation of the palatal root with BC Putty and sealer (D) Post-surgical radiograph (E – F) pre-operative scan images showing large through-and-through lesion extending to the palatal root. (G – H) 2 yrs. follow up scan images showing complete healing of the DB and palatal roots.
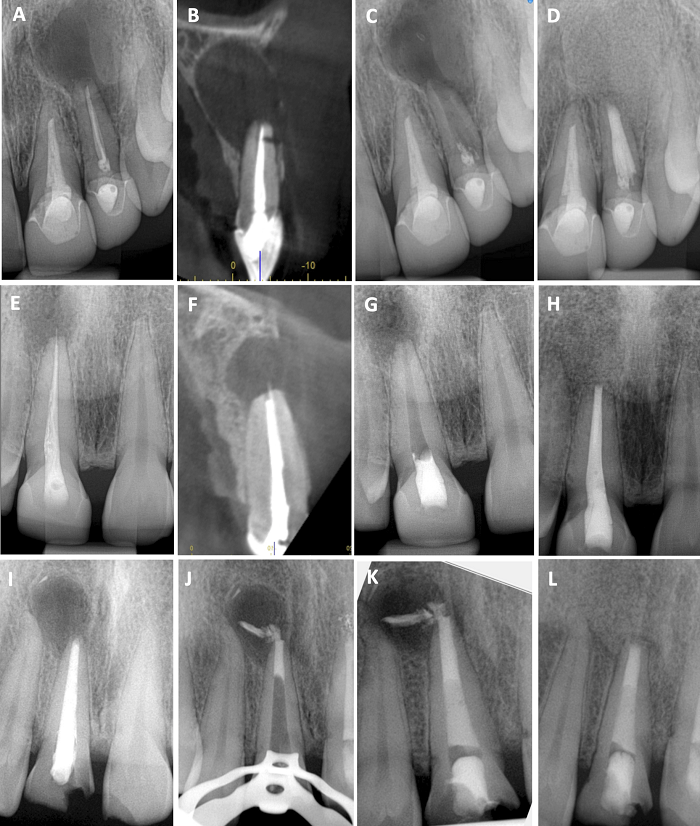
Figure 4: demonstration of 3 different surgical management approaches of maxillary anterior teeth with poor RCT and no coronal obstruction.
Option 1 (A-D): complete surgical retreatment using long retro-preparation. Post-op radiograph showing excessive damage of the root of the lateral incisor from the long preparation.
Option 2 (E – H): RET and no obturation followed by surgical intervention and filling the entire root during the surgery
Option 3 (I – L): RET and sealing of the apical 5mm with a root repair material, followed by obturation and apical resection.
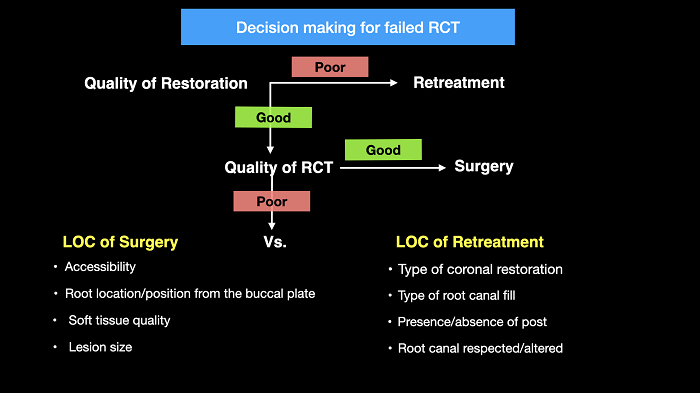
Figure 5: A flowchart describing the decision-making process in failed endodontic treatments.
LOC = level of complexity
References
- Friedman S. Retrograde approaches in endodontic therapy. Endod Dent Traumatol 1991;7:97-107.
- Setzer FC, Shah SB, Kohli MR, Karabucak B, Kim S. Outcome of endodontic surgery: a meta-analysis of the literature–part 1: Comparison of traditional root-end surgery and endodontic microsurgery. J Endod 2010;36:1757-65.
- Torabinejad M, Landaez M, Milan M, Sun CX, Henkin J, Al-Ardah A, et al. Tooth retention through endodontic microsurgery or tooth replacement using single implants: a systematic review of treatment outcomes. J Endod 2015;41:1-10.
- Kruse C, Spin-Neto R, Christiansen R, Wenzel A, Kirkevang LL. Periapical Bone Healing after Apicectomy with and without Retrograde Root Filling with Mineral Trioxide Aggregate: A 6-year Follow-up of a Randomized Controlled Trial. J Endod 2016;42:533-7.
- Curtis DM, VanderWeele RA, Ray JJ, Wealleans JA. Clinician-centered Outcomes Assessment of Retreatment and Endodontic Microsurgery Using Cone-beam Computed Tomographic Volumetric Analysis. J Endod 2018;44:1251-6.
- Ng YL, Mann V, Gulabivala K. Tooth survival following non-surgical root canal treatment: a systematic review of the literature. Int Endod J 2010;43:171-89.
- Torabinejad M, White SN. Endodontic treatment options after unsuccessful initial root canal treatment: Alternatives to single-tooth implants. Journal of the American Dental Association 2016;147:214-20.
- Ricucci D, Siqueira JF, Jr. Biofilms and apical periodontitis: study of prevalence and association with clinical and histopathologic findings. J Endod 2010;36:1277-88.
- Siqueira JF, Jr., Lopes HP. Bacteria on the apical root surfaces of untreated teeth with periradicular lesions: a scanning electron microscopy study. Int Endod J 2001;34:216-20.
- Ricucci D, Loghin S, Goncalves LS, Rocas IN, Siqueira JF, Jr. Histobacteriologic Conditions of the Apical Root Canal System and Periapical Tissues in Teeth Associated with Sinus Tracts. J Endod 2018;44:405-13.
- Ng YL, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: part 1: periapical health. Int Endod J 2011;44:583-609.
- Hirshberg A, Tsesis I, Metzger Z, Kaplan I. Periapical actinomycosis: a clinicopathologic study. Oral surgery, oral medicine, oral pathology, oral radiology, and endodontics 2003;95:614-20.
- Nair PN. On the causes of persistent apical periodontitis: a review. Int Endod J 2006;39:249-81.
- Nair PR, Pajarola G, Schroeder HE. Types and incidence of human periapical lesions obtained with extracted teeth. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 1996;81:93-102.
- Gorni FG, Gagliani MM. The outcome of endodontic retreatment: a 2-yr follow-up. J Endod 2004;30:1-4.
- von Arx T, Maldonado P, Bornstein MM. Occurrence of Vertical Root Fractures after Apical Surgery: A Retrospective Analysis. J Endod 2021;47:239-46.
- Azim AA, Albanyan H, Azim KA, Piasecki L. The Buffalo study: Outcome and associated predictors in endodontic microsurgery- a cohort study. Int Endod J 2021;54:301-18.
- Tawil PZ, Arnarsdottir EK, Phillips C, Saemundsson SR. Periapical Microsurgery: Do Root Canal-retreated Teeth Have More Dentinal Defects? J Endod 2018;44:1487-91.
- Tawil PZ. Periapical Microsurgery: Can Ultrasonic Root-end Preparations Clinically Create or Propagate Dentinal Defects? J Endod 2016;42:1472-5.
- Tawil PZ, Saraiya VM, Galicia JC, Duggan DJ. Periapical microsurgery: the effect of root dentinal defects on short- and long-term outcome. J Endod 2015;41:22-7.
- Safi C, Kohli MR, Kratchman SI, Setzer FC, Karabucak B. Outcome of Endodontic Microsurgery Using Mineral Trioxide Aggregate or Root Repair Material as Root-end Filling Material: A Randomized Controlled Trial with Cone-beam Computed Tomographic Evaluation. J Endod 2019;45:831-9.
- Azim AA, Wang HH, Serebro M. Selective Retreatment and Sinus Lift: An Alternative Approach to Surgically Manage the Palatal Roots of Maxillary Molars. J Endod 2021;47:648-57.




