Cracking the Cracked Tooth Code: From Unpredictability to Predictability
By Mohamed I. Fayad, D.D.S., M.S., Ph.D., with contributor Bradford R. Johnson, D.D.S.
The purpose of this Communique article is to review advances in CBCT imaging and a new software, e-Vol DX, for early diagnosis of cracked teeth, marginal ridge cracks (MRC), and vertical root fractures (VRF), as well as new advances in restorative dentistry to restore teeth presenting with MRC. Cracked teeth can present a diagnostic challenge, a restorative dilemma, and often a source of frustration for both clinicians and patients because of the vague symptoms, low sensitivity of available imaging modalities, and unpredictable prognosis. Problems related to cracked teeth are the third leading cause of tooth loss after caries and periodontal disease. (1)
Cracks and root fractures generally develop slowly over time. By the time a crack is visible, it has progressed through three stages: initiation, propagation, and manifestation. Once a crack has initiated, it can remain asymptomatic for several years. An asymptomatic phase can change drastically over time as the crack is subjected to repetitive parafunctional habits, (2, 3) occlusal stress, thermal cycling and colonization with bacterial biofilms (4).
Cracked teeth may present with crack lines present in the vertical plane. Several terminologies and classifications have been proposed to describe the characteristics of cracked teeth. The American Association of Endodontists (AAE) categorizes cracks into five types: craze lines, fractured cusp, cracked tooth, split tooth and vertical root fracture (VRF). The term longitudinal fracture is used because it typically represents vertical extension of fractures over distance and time. These five categories of longitudinal fractures have been devised to provide global definitions that researchers and clinicians can use to make the various conditions more widely understandable (5). This issue of Communique will focus on MRC and VRF.
Cracked teeth are diagnosed based on clinical manifestations and clinical exam testing such as, transillumination, periodontal probing depths, biting stress test, magnification, and staining with methylene blue. Although these tests are useful, there is no standard examination that can predict the long-term outcome of cracked tooth treatment. The AAE Colleagues for Excellence classified treatable versus untreatable cracked teeth based on longitudinal marginal ridge crack extension apically into the root in relation to the cementoenamel junction (CEJ). The ability to assess the apical extent of a MRC would be a great diagnostic aid for clinicians to support case selection and clinical decision-making.
Assessment of the extent of a MRC is critical for predicting the most likely treatment outcome. For years, endodontists were accustomed to evaluating the internal extent of the MRC using methylene blue staining and operating microscopes. On the other hand, the external extension of the MRC on the root surface was proposed to be a more accurate predictor of the prognosis of a MRC tooth and would allow clinicians to make a better pre-treatment decision regarding treatment outcome (6). Alternative radiographic imaging systems have recently become available for use in dentistry. Among these new imaging technologies is cone-beam computed tomography (CBCT). CBCT technology allows the precise visualization and evaluation of teeth and the surrounding structures. The use of CBCT has great potential as a diagnostic tool to assist in the detection of the external extent of MRC and vertical root fractures by detecting early patterns of bony changes adjacent to the MRC and VRF.
A Joint Position Statement by the American Association of Endodontists and the American Association of Oral and Maxillofacial Radiologists (AAE/AAOMR) recommends CBCT as the imaging modality of choice for such cases (7).
CBCT imaging has the diagnostic capability to detect early patterns of bony changes adjacent to marginal ridge cracks and vertical root fractures. Based on these early patterns of bony changes, the clinician can determine the extension of the MRC on the external surface of the root and its location prior to initiating treatment. If left untreated, the MRC will propagate on the external surface of the root and will result in breakdown of periodontal attachment and periodontal defect formation.
Despite technological advancements in CBCT hardware, the interpretation of the acquired images is still compromised by viewing software packages that often have limited navigational tools and lack adequate filters to overcome some challenges of CBCT technology such as artifacts. A new CBCT software package (e-Vol DX, CDT- Brazil) has been developed to overcome these software limitations and support diagnosis, treatment planning, and management of endodontic cases (8). This imaging method provides high resolution images due to submillimeter voxel sizes, dynamic multi-plane imaging navigation, the ability to change the volume parameters such as slice thickness and slice intervals, and data correction applying imaging filters and manipulation of brightness and contrast. With e-Vol DX, clinicians can visualize marginal ridge crack extension in relation to the CEJ as well as vertical root fractures for the first time (Figure 1).
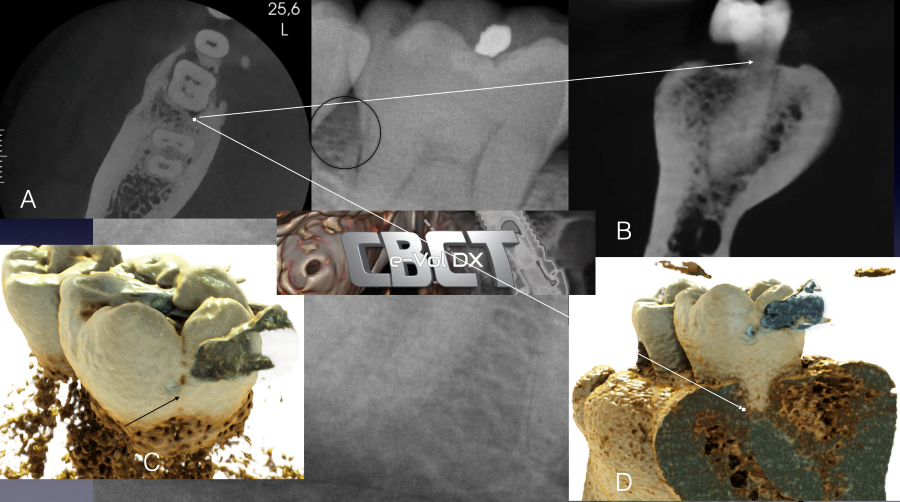
Figure 1: Tooth #30 presents with a distal marginal ridge crack. The periapical radiograph demonstrated normal distal root bone pattern and periodontal probings were within normal limits (WNL) (a) Axial CBCT view demonstrating the distal bony changes adjacent to the distal marginal ridge crack. (b) CBCT DICOM images imported into e-VolDX software and utilizing the fracture filter. The distal marginal ridge crack extending below the CEJ can be visualized. (c and d) Applying the realistic rendering function and visualizing the distal marginal ridge crack extension as well as the early distal bony changes adjacent to the distal marginal ridge crack. All views confirm that the distal marginal ridge crack has extended below the CEJ.
The combination of early patterns of bony changes and the actual visualization of the MRC extension as well as VRF has been a breakthrough in CBCT imaging providing the clinician with more accurate 3-D information. Based on this enhanced information, the clinician can make an accurate diagnosis, leading to a more predictable outcome. (Figures 2 and 3)
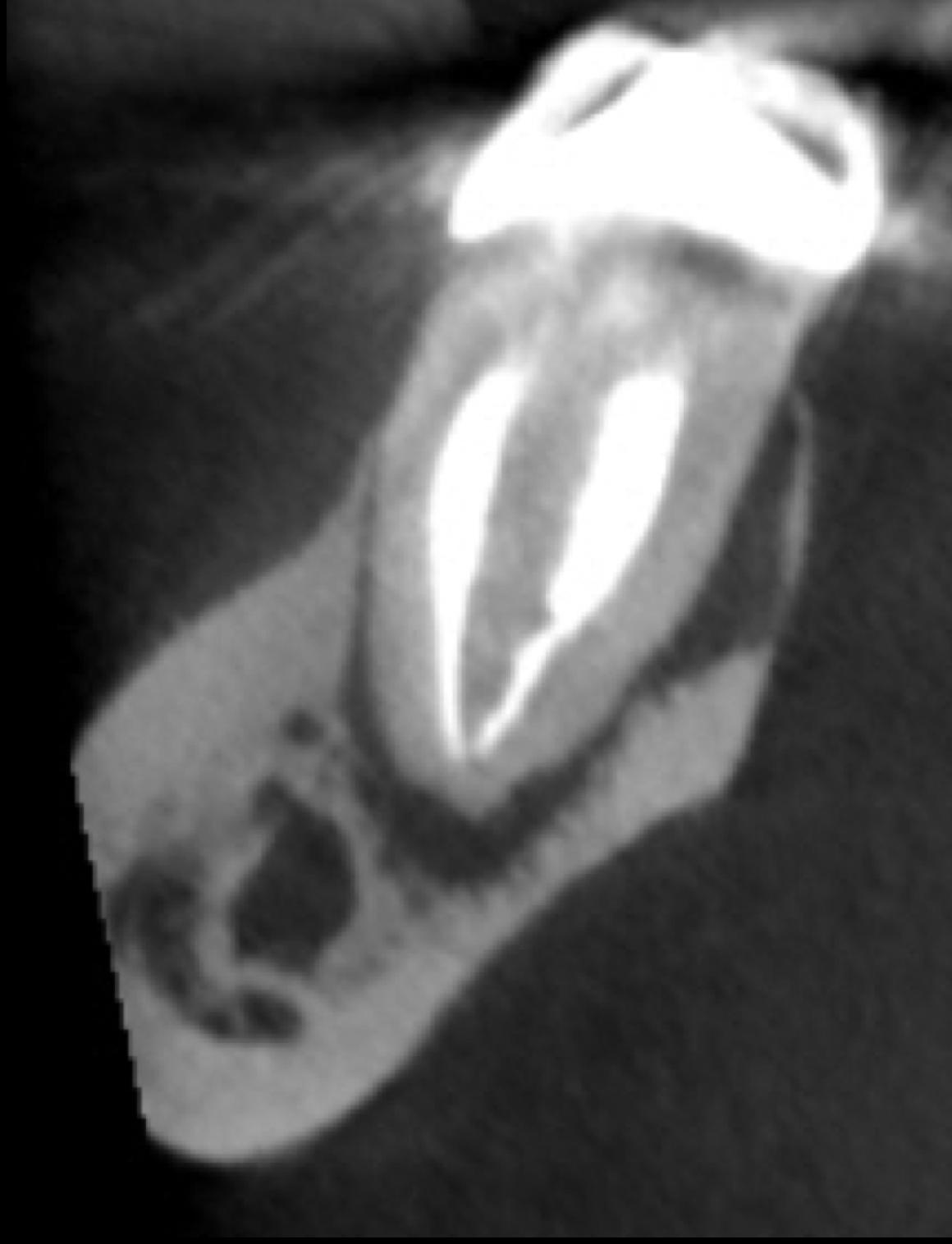
Figure 2: Tooth # 30 was referred for non-surgical / surgical re-treatment. The coronal view demonstrated a low-density area associated with the root apex as well as early bone changes adjacent to the lingual aspect of mesial root. At the time of the clinical examination, the lingual aspect of the mesial root presented with no abnormal periodontal probings due to the intact lingual collar of bone.
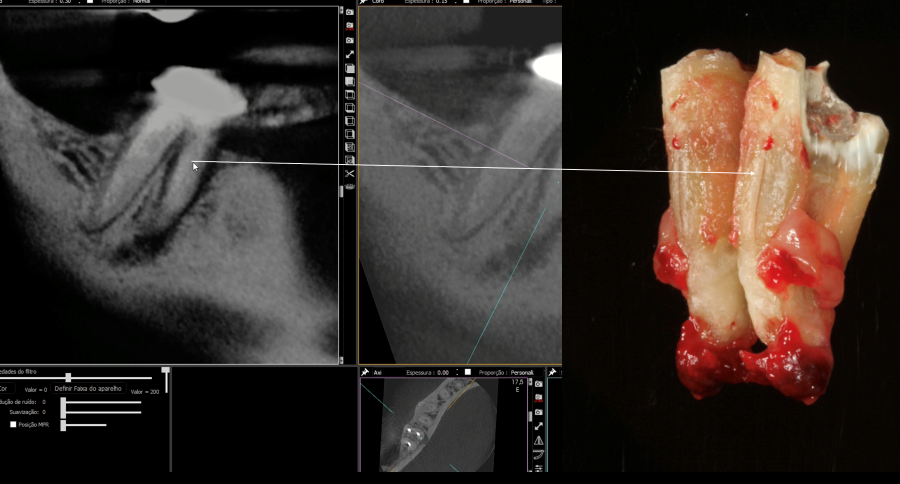
Figure 3: DICOM CBCT images imported into e-VolDX software and utilizing the fracture filter. The lingual VRF of the mesial root can be visualized and coincides with the VRF present on the lingual root after tooth #30 was extracted. Note the fine size of VRF on the extracted mesial root and the sensitivity of the e-VolDX filter demonstrating the VRF.
When teeth present with MRCs that are considered treatable, it is generally accepted that early restorative intervention is recommended to prevent irreversible damage, such as pulpal inflammation/necrosis and/or structural failure. Historically, various forms of dental intervention from occlusal adjustment to indirect and direct restorations, to orthodontic bands have been advocated. Although many options have been proposed for the treatment of posterior MRC, most of the treatment recommendations are not evidence based. In a study that evaluated the differences in treatment approach of dental practitioners toward different cracked teeth scenarios, a large difference in the approach and treatment planning between dental practitioners and specialists was observed (9). Although, there are no universally accepted restorative protocols, the aim of restorative therapy is to immobilize the segments of the tooth that flex on loading (10).
Improved understanding of the microanatomy of tooth structure has led to a revolution in dentistry that is known by several names, including micro dentistry, minimally invasive dentistry, biomimetic dentistry, and bio emulation dentistry. These treatment concepts have developed due to a coalescence of principles of tooth microanatomy, materials science, adhesive dentistry, and reinforcing techniques that, when applied together, will allow dentists to predictably repair and restore teeth. Evidence now supports the concept that the enamel on a tooth acts like a compression dome protecting the underlying dentin from damaging tensile forces (compression dome concept). Disruption of the compression system, such as MRC, leads to significant shifts in occlusal loads resulting in crack propagation, flexural pain, and fracture loss of tooth structure (11). Figure (4 ) is an example of the new compression dome concept of restoring teeth with MRCs.

Figure 4: Compression dome adhesive ceramic onlay. This onlay design aims to retain circumferential enamel above the inflection plane (height of contour), creating a stable peripheral bond in conjunction with the compressive design.
Teeth with MRC can present as asymptomatic or symptomatic. To date, studies have evaluated the prognosis of symptomatic cracked teeth and cracked teeth that were retained by endodontic treatment. Clinical outcomes of cracked teeth diagnosed with reversible pulpitis were evaluated (12). It was concluded that if marginal ridge cracks were identified early enough in teeth diagnosed with reversible pulpitis and a crown was placed, root canal treatment was necessary in only about 20% of the cases within a 6-month period. A similar study evaluated pulpal complications after diagnosis of vital cracked teeth (13). Fifty-eight out of 199 (29.1%) teeth had pulpal complications. Thirty-eight of 58 (65.5%) were diagnosed with irreversible pulpitis after 1.2 years, and 20 of 58 (34.5%) were diagnosed with necrotic pulp after 2 years. It was concluded that the absence of a full-coverage crown increased the risk of pulpal complications. These studies confirm that it is essential to brace the cracked tooth to minimize cusp flexion and to provide full coverage that will protect the structural integrity and protect the pulp from the oral environment and bacterial contamination of the pulp.
The outcome and survival of endodontically treated cracked posterior teeth was evaluated in several recent studies (14, 15). One study concluded that success and survival rate for cracked teeth ranged between 90 to 100%, respectively, with a follow-up period of 2–4-years (15). Studies evaluating the success and survival rates of endodontically cracked teeth without a pre-operative CBCT is a major limitation in most studies. The results of the previous studies can be skewed dramatically based on the unknown external extension of the MRC.
In summary, the prognosis for teeth with MRCs is determined by three principal factors: the extent and location of the crack, the point in time when restorative intervention is initiated, and the type of restoration. For teeth presenting with MRCs, early restoration with full cuspal coverage can improve the outcome. MRCs above the CEJ junction may be predictably treated, whereas radicular cracks extending below the CEJ have a lower prognosis with an increased probability of extraction (16). Teeth presenting with MRCs are more often lost due to periodontal breakdown than structural failure. For cracked teeth presenting with irreversible pulpitis, research has shown that endodontic treatment is an option and has a favorable prognosis when the MRC has not extended below the CEJ. CBCT imaging and new software such as e-Vol DX aids in diagnosis and treatment planning for teeth with MRCs and VRFs.
References:
- Hilton T, Ferracan J. Cracked Teeth Registry. National Dental PBRN Western Regional Meeting. September 28, 2013.
- Ellis SG. Incomplete tooth fracture-proposal for a new definition. Br Dent J 2001;190:424-8.
- Lynch CD, McConnell RJ. The cracked tooth syndrome. J Cand Dent Assoc 2002:68:470-5.
- Ricucci D, Siqueira JF, Loghin S. The cracked tooth: histopathologic and histobacteriologic aspects. J Endod 2015;41:343-52.
- American Association of Endodontists. Cracking the cracked tooth code. Endodontics: Colleague of Excellence. Chicago: American Association of Endodontists;2008.
- Chen M, Fu K, Qiao F. et al. Predicting extension of cracks to the root from the dimensions in the crown. JADA 2017:148:737-42.
- AAE and AAOMR Joint Position Statement: Use of Cone Beam Computed Tomography in Endodontics 2015 Update. J Endod 2015;41:1393-6.
- Bueno M, Estrela C, Azevedo B, Diogenes A. Development of a new Cone-Beam Computed Tomography software for endodontic diagnosis. Braz Dent J 2018;29(6):517-29.
- Alkhalifah S, Alkandari H, Sharma N P, Moule J A. Treatment of cracked teeth. J Endod 2017;43(9):1579-86.
- Banerji S, Mehta B, Millar J B. Cracked tooth Syndrome. Part 2: restorative options for the management of cracked tooth syndrome. Br Dent J 2010;208:503-14.
- Milicich G. The compression dome concept. The restorative implications. AGD 2017;55-60.
- Krell KV, Rivera E. A six year evaluation of cracked teeth diagnosed with reversible pulpitis: Treatment and prognosis. J Endod 2007;33(12):1405-07.
- Wu S, Lew H, Chen N. Incidence of pulplal complications after diagnosis of vital cracked teeth. J Endod 2019;1-5.
- Olivieri JG, Elmsmari F, Miro Q, Ruiz XF, Krell KV, Garcia-Font M, et al. Outcome and Survival of endodontically treated cracked posterior permanent teeth: A systemic review and meta-analysis. J Endod 2020;46:455-63.
- Davis MC, Shariff SS. Success and survival of endodontically treated cracked teeth with radicular extensions. A 2-4-year prospective cohort. J Endod 2019;45:848-55.
- Sim G.B.I, Lim T, Chen N. Decision making for retention of endodontically treated posterior cracked teeth. A 5-year follow-up study. J Endod 2016;42:225-29.




